
PCOS symptoms: The full list and what they mean
Experiencing irregular periods, new hair growth on your body, or difficulty losing weight? All are potential PCOS symptoms—though they aren’t the only potential signs of PCOS and they could be due to other medical conditions. Here’s a comprehensive list of the potential symptoms of PCOS, plus how to decipher if PCOS or another condition is the culprit.
Polycystic ovary syndrome (PCOS) is a common hormonal condition. Stats on prevalence vary, but as many as one in five people who menstruate have PCOS. While there are some symptoms we often associate with it (fertility problems, irregular periods, acne, etc.), PCOS looks different for everyone, which is part of why it’s underdiagnosed.
“PCOS is complex, and the condition as a whole comes in many different forms and symptoms,” says Gouri Pimputkar DO FACOOG, DipABLM, clinical lead at Allara Health., “Patients with PCOS can often be dismissed because they don’t fit the mold.”
To make matters more confusing, symptoms may also stem from other medical conditions, which is why seeing the right specialist who can conduct PCOS testing is so important. But before you make that appointment, let’s review what the symptoms of PCOS look like and how to tell them apart from other conditions.
What are the symptoms of PCOS?
PCOS is a common reproductive health disorder (or, in medical speak, an endocrine condition). It’s characterized by a hormonal imbalance, usually manifesting as higher levels of androgens ( male sex hormones) than necessary for someone who menstruates.
To be diagnosed with PCOS, someone must meet at least two of the three Rotterdam Criteria:
- Clinical or biochemical evidence of excess male hormones (referred to as hyperandrogenism)
- Evidence of “oligo-anovulation,” which is when ovulation is irregular
The first two criteria can be tricky to determine, since that “evidence” can look different for everyone. While we often think of PCOS as a fertility issue or a reproductive health issue, the evidence shows up throughout the body.
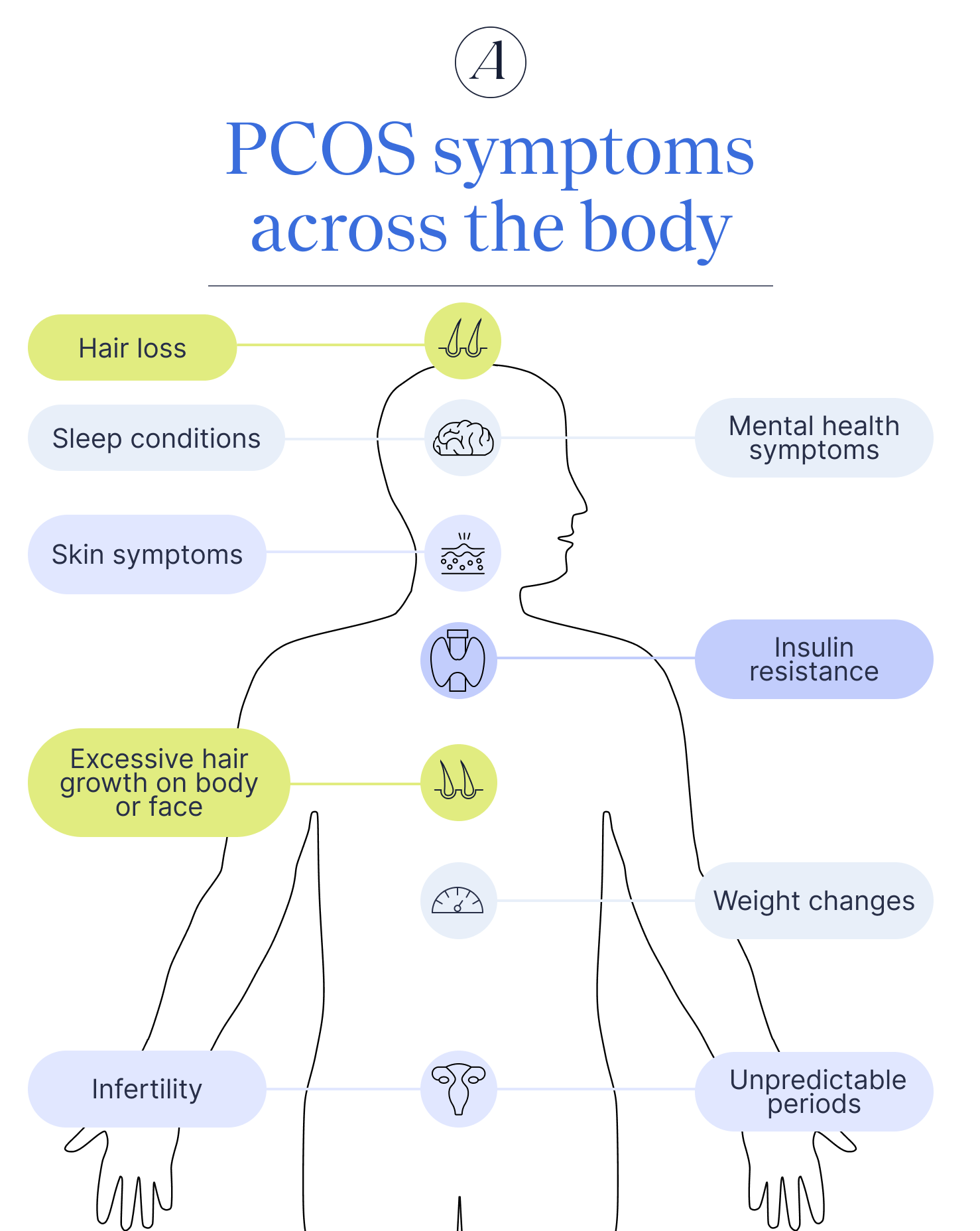
Excessive male hormones, for example, may take the shape of excessive body hair growth, skin symptoms, or even insulin resistance (which sounds unrelated, but we promise to explain later). Oligo-anovulation usually looks like irregular periods, but may also result in infertility or painful periods.
Why do PCOS symptoms vary so much?
Someone’s environment, lifestyle, genetics, and metabolism all impact what PCOS feels like. Dr. Pimputkar explains, “PCOS comes in all different shapes and sizes, and there are different presentations of the condition.”
She points out that while PCOS symptoms vary, most patients fit into one of four typical subcategories:
- Phenotype A: One of two “classic” phenotypes that presents with a lot of the symptoms we most commonly associate with PCOS. Think: menstrual irregularities, signs of excessive male sex hormones, and weight changes. Signs of polycystic ovaries also show up on ultrasounds with this type.
- Phenotype B: As the other “classic” phenotype, this subcategory presents with the same symptoms as phenotype A. The main difference is that there aren’t polycystic ovaries.
- Phenotype C: This subcategory features signs of excessive male sex hormones and polycystic ovaries show up on ultrasounds. However, ovarian function is not impacted, meaning someone with this phenotype will have more regular menstrual cycles.
- Phenotype D: When someone has this phenotype, they don’t present symptoms of excessive male sex hormones. They do have symptoms of oligo-anovulation, and polycystic ovaries show up on ultrasounds.
Menstrual, ovulatory, and fertility-related symptoms
When you think of PCOS, the first symptoms that come to mind probably relate to reproductive health. These include PCOS period symptoms, like irregular menstruation or painful periods, and issues with fertility.
Irregular or missed periods
When someone has PCOS, their male sex hormone levels are too high. At the same time, there’s an “abnormal expression of estrogen” within the ovaries. Together, these two hormonal changes disrupt the menstrual cycle. Often, the first sign of that interference is skipped or irregular periods.
“Typically patients with PCOS have issues with irregular periods,” says Dr. Pimputkar, “Periods can be spaced out for months at a time or occurring at different times each month.” This can make it hard to track your menstrual cycle—and yes, that may also lead to anxiety or dread when a period is late or missing.
Painful periods
PCOS pain is a very real symptom, though it’s not as common as menstrual irregularities. In one study, almost 30% of people with PCOS reported pain, with cramping during periods being the most reported type.
The reason for painful periods relates back to how PCOS disrupts the menstruation. While periods are the most evident part of this cycle, the high androgen levels may mean your ovaries don’t release eggs as intended. This allows the uterine lining to build up over time.
When you menstruate, the body releases prostaglandins to help the wound contract and release this lining. The shedding of the lining is what causes your period. If the lining is thicker, the body will release more prostaglandins, increasing the contractions and potentially causing pain.
Heavy periods
A heavy flow may point toward PCOS. As many as 70% of people with PCOS report heavy bleeding during their menstrual cycle. This is because your period is the body’s release of the uterine lining—and a thicker lining, which PCOS can cause, means a heavier flow.
Follicles on the ovaries
The “cystic” in polycystic ovary syndrome actually refers to follicles measuring 2-9mm in the ovaries. Cysts are larger sacs filled with fluid that can naturally occur during menstruation. The prefix poly means “much or many” in Greek. When you combine the two together, polycystic refers to enlarged follicles, which are one of the three Rotterdam criteria.
These cysts show up on ultrasounds but are often hard to detect in everyday life since they’re usually symptomless. When they do cause symptoms, they often take the shape of PCOS bloating and abdominal or pelvic pain. Even though these enlarged follicles are, not all cysts are a sign of PCOS—yet another reason it’s important to see a PCOS specialist, such as an endocrinologist or a gynecologist.
Infertility and irregular ovulation
Along with skipped or irregular periods, someone may also experience anovulatory periods, which is when there’s a monthly flow but no ovulation. This is associated with infertility, one of the most talked about symptoms of PCOS.
Yet frequently talked about does not equal most common. About 70% of people with PCOS experience oligo-anovulation, which is associated with, but does not always lead to, infertility. That means for 30% of people with PCOS, infertility isn’t a symptom. For the remaining 70%, they are more likely to experience difficulties getting pregnant, but infertility should not be assumed with PCOS.
If someone is susceptible to infertility, working with a reproductive health specialist can help. A specialist can recommend fertility medications and lifestyle changes, such as following a healthy diet or a reduction in body weight, which can increase the likelihood of getting pregnant.
Hormonal and metabolic symptoms
As a hormonal health condition, PCOS impacts parts of the body beyond the reproductive system. This can take the shape of metabolic symptoms, such as weight changes and insulin resistance.
Insulin resistance
Insulin is a hormone created by the pancreas. It helps blood glucose, aka blood sugar, enter cells in the liver, muscles, and fat. These cells then use insulin for energy. If cells become desensitized to insulin (think: type 2 diabetes), blood sugar levels remain too high for too long. This may lead to a variety of health impacts, including permanent damage to the eyes and nerves. It can also be life-threatening if left untreated.
Many factors increase the risk of insulin resistance, including PCOS. In fact, over 50% of people with PCOS will develop type 2 diabetes before they turn 40. However, it’s important to note there is a strong correlation, not causation, and researchers are still studying if PCOS causes insulin resistance or vice versa.
Weight changes
“Weight gain is also very common with patients who suffer from PCOS,” says Dr. Pimputkar, “This is because PCOS is very much a metabolic condition, in addition to a hormonal condition.”
We can think of hormones like messengers. They deliver messages throughout the body, including to our metabolic system. With PCOS specifically, higher androgen levels may disrupt signals that help with appetite regulation and the process of turning food into energy. Food that isn’t converted to usable energy typically becomes fat and when our appetite isn’t regulated, we may eat more than necessary.
Together, the two effects can make it hard to drop unwanted pounds. The metabolic effects of PCOS may also mean someone gains weight more easily.
Plus, PCOS’ relationship with insulin resistance also plays a role in weight management. Dr. Pimputkar explains, “The insulin metabolism can be affected by the hormonal changes happening at the level of the ovary, which can lead to weight gain and set off a whole cascade of other conditions like high cholesterol, diabetes, and heart disease.”
Digestive symptoms
PCOS affects hormones throughout the body, including those in the gut. This means people with PCOS often have a higher risk of certain gastrointestinal conditions, such as irritable bowel syndrome (IBS). GI conditions often lead to digestive symptoms like constipation, diarrhea, and bloating.
Skin and hair symptoms
“Patients with PCOS can have complaints of an increase in hair growth in unwanted places or hair loss, hair thinning, as well as acne,” explains Dr. Pimputkar, “All of which is usually a signal of excess androgen or testosterone production.”
Skin symptoms
Skin PCOS symptoms can be one of the first signs of PCOS. The exact ways PCOS impacts skin health varies, though some of the most common skin symptoms are:
- Acne breakouts
- Oily skin
- Hyperpigmentation or dark patches of skin (on face or body)
- PCOS skin tags
- Facial redness
Excessive facial or body hair growth
Hyperandrogenism may also lead to hair growth patterns that are more common in people assigned male at birth. This often includes excessive hair growth on the face or body. Hirsutism, facial hair growth in those who menstruate, is especially common. PCOS contributes to upwards of 72% of hirsutism cases.
Hair loss on the scalp
Ironically, too many androgens leads to hair loss as well as hair growth. More specifically, it leads to thinning hair on the scalp. This is referred to as androgenetic alopecia (aka female pattern hair loss).
Mental health and neurological symptoms
Remember how hormones are messengers? Turns out, the brain is on their delivery route too. PCOS’ hormonal impacts can impact mental health—and that’s before we talk about the emotional impact of dealing with PCOS’ physical symptoms.
Mood swings
PCOS creates the perfect storm for mood swings, thanks to three distinct reasons:
- Hormonal disruptions: PCOS may lead to the dysregulation of progesterone, serotonin, and estrogen. Among other roles, these hormones help people who menstruate regulate their mood.
- Inflammation: PCOS is also a low-grade inflammatory condition. Inflammation may lead to increased irritability and other mood disruptions because it impacts how the brain responds to stress and other emotional triggers.
- Dealing with other symptoms: Last but certainly not least, dealing with PCOS symptoms as a whole can be mentally challenging. Stress over missed periods, difficulty managing weight, PCOS acne, and more can all make you feel more anxious than desired.
Mental health conditions
Thanks to PCOS mood swings, those with PCOS are at a higher risk for various mental health conditions. For instance, people with PCOS are 2.5 times more likely to experience depression than people without it. Another study suggests 42% of people with PCOS experience anxiety symptoms, compared to 8.5% in people without PCOS.
Eating disorders are also more likely to occur. The most common in people with PCOS is binge eating disorder (BED), which is marked by eating large amounts of food in a short time. The increase in eating disorders might be an emotional response to PCOS’ impact on weight, though research is not conclusive on why this association exists.
Sleep disturbances
PCOS may also disrupt sleep for a few reasons. First, co-existing PCOS and depression may lead to hypersomnia, sleeping too much, or insomnia, sleeping too little. Progesterone also plays a role in regulating sleep—and PCOS messes with progesterone levels. Several hormonal disruptions arethe most likely reason why there’s an extremely strong link between PCOS and insomnia.
PCOS also increases the risk of being overweight or obese. Either of these weight-related conditions may lead to obstructive sleep apnea, a condition where difficulty breathing wakes someone up throughout the night.
Fatigue and low energy
People with PCOS are more likely to report low energy than those without PCOS. Researchers aren’t exactly sure why PCOS fatigue occurs, though it may be linked to trouble sleeping, as well as PCOS’ impact on insulin and blood sugar levels.
Less common and often overlooked PCOS symptoms
While the above list is pretty comprehensive, it doesn’t encompass all symptoms of PCOS. Headaches, pelvic pain, and Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) are associated with PCOS, though that doesn’t necessarily mean PCOS causes them. In the case of NAFLD, for example, the correlation stems from obesity, which PCOS is a risk factor for.
PCOS increases the risk for some endometrial and uterine cancer when other risk factors are present too. Dr. Pimputkar explains, “For patients who do not have periods regularly, combined with other risk factors, there can also be an increased risk of pre-cancer cells in the uterus eventually leading to endometrial/uterine cancer.”
Some studies also suggest a correlation between PCOS, blood clots, and deep vein thrombosis, though other studies do not find that link. All this goes to say that the jury’s still out on PCOS’ full list of symptoms.
PCOS symptoms that overlap with other conditions
As if PCOS varying symptoms weren’t enough, the hallmark signs of PCOS may also stem from other conditions. Overlapping conditions include thyroid disorders, endometriosis, perimenopause, and functional hypothalamic amenorrhea (FHA).
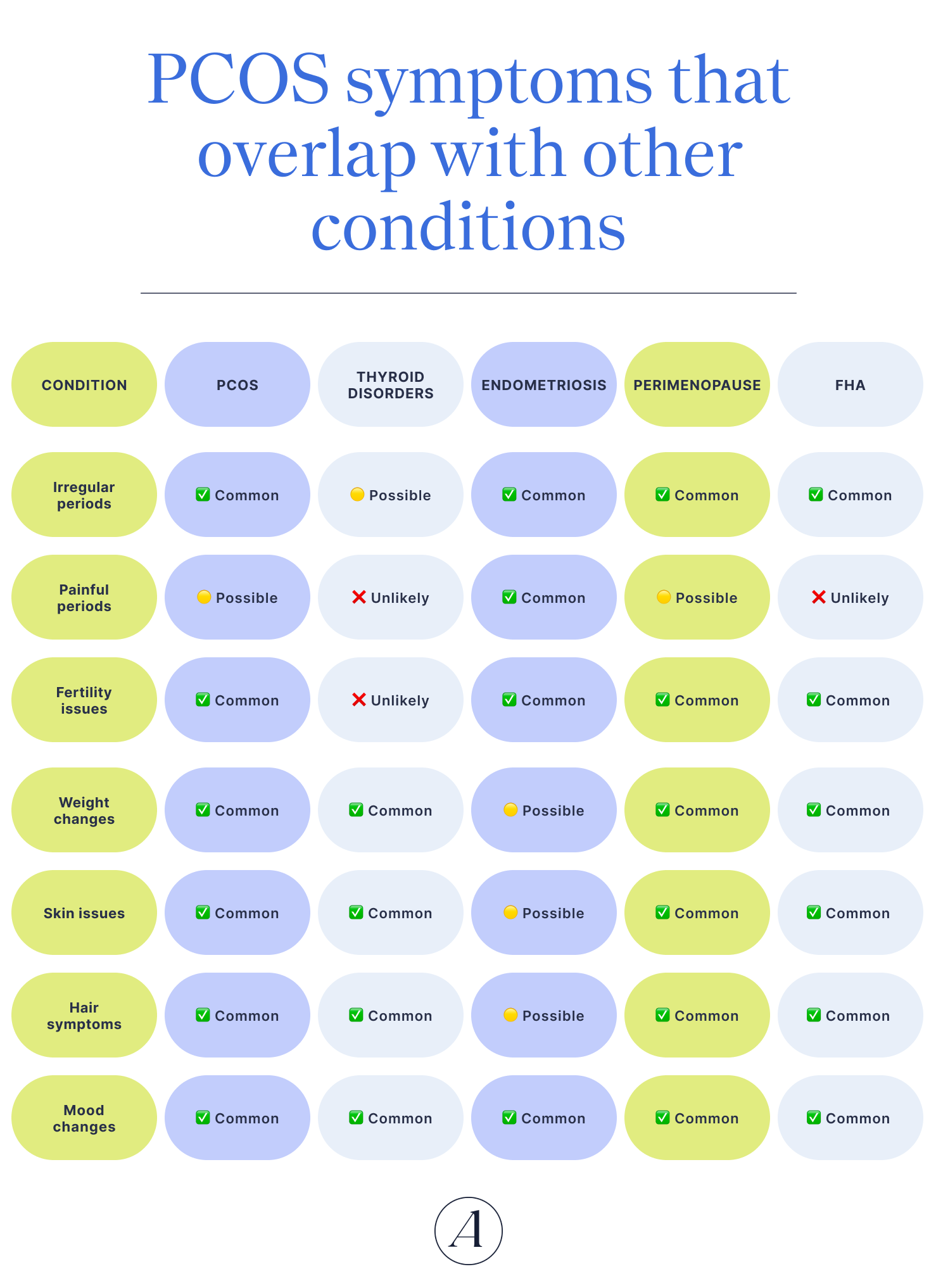
Thyroid disorders
- What it is: “Disorders of the thyroid can also give irregular periods, infertility, hyperandrogen symptoms, and weight gain,” says Dr. Pimputkar. While they are different from PCOS, thyroid disorders are likely to co-occur with PCOS.
- Overlapping symptoms: Menstrual irregularities, weight gain, excessive hair growth, hair loss on scalp, and low energy
- Key difference: Thyroid disorders don’t cause cystic ovaries.
Endometriosis
- What it is: Endometriosis is a condition where cells similar to the lining of the uterus grow in other parts of the body. It can cause some of the same symptoms as PCOS, with significant overlap in how the two impact reproductive and mental health.
- Overlapping symptoms: Infertility, irregular periods, heavy bleeding, and mood changes
- Key differences: Endometriosis is due to abnormal tissue growth while PCOS is hormonal. Endometriosis is also more likely to cause pain, and that pain is often more severe than with PCOS.
Perimenopause
- What it is: Perimenopause is the transition from having a menstrual cycle to not having one. When someone hasn’t had a menstrual cycle for 12 consecutive months, it’s referred to as menopause. Perimenopause creates similar hormonal imbalances as PCOS, resulting in many of the same symptoms.
- Overlapping symptoms: Irregular periods, weight changes, mood changes, acne, sleep disturbances, hair changes, and infertility
- Key difference(s): Perimenopause is a natural transition whereas PCOS is a hormonal disorder.
Functional hypothalamic amenorrhea (FHA)
- What it is: This condition occurs when stress levels, physical activity, or eating disorders lead to a disruption or absence of the menstrual cycle. FHA presents many of the same symptoms as PCOS, though FHA is usually caused by disordered eating, exercising too much, and/or psychological stress.
- Overlapping symptoms: Irregular periods, cystic ovaries on ultrasounds, insulin resistance, weight changes, acne, hair changes, mood issues, and fatigue
- Key difference(s): While PCOS is a hormonal and metabolic condition, FHA stems from stress, eating disorders, or overexercise.
What to do if you recognize these symptoms
Recognizing these symptoms is only half the battle. Since they overlap with other conditions, it’s hard (insert: impossible) to DIY a PCOS diagnosis. Instead, the first step when symptoms occur is to make an appointment with a PCOS specialist and advocate for yourself.
“Advocate for yourself and do not settle for this is ‘just how it is,’” says Dr. Pimputkar. This often looks like making an appointment with a healthcare provider who has experience treating PCOS, such as the team at Allara. From there, they can conduct a thorough hormonal evaluation, as well as order any imaging that can help present a clearer picture.
Before the appointment, track symptoms, including when they take place and what they feel like. In particular, pay attention to your monthly cycle. “Our periods should be considered a vital sign,” says Dr. Pimputkar, “If periods start becoming irregular or other symptoms become more prominent, it is time to have a discussion with your provider.”
The bottom line
- PCOS can cause a variety of symptoms, including hair and skin changes, disruptions to the menstrual cycle, infertility, mood swings, fatigue, insulin resistance, and weight changes.
- Not everyone with PCOS experiences every symptom. The condition looks different for everyone, and other conditions, including endometriosis, thyroid disorders, perimenopause, and FHA, can also cause many of these symptoms.
- Because of the many, many possible symptoms and the overlap with other conditions, it’s important to see a reproductive health specialist to determine the underlying cause. That specialist can also help manage PCOS symptoms.
- At Allara Health, our team of specialists create comprehensive treatment plans that treat the whole you and provide ongoing support.
Frequently asked questions (FAQs)
What are the first signs of PCOS?
The first signs of PCOS are different for everyone. Some people experience irregular or skipped periods first. Others report the first signs are acne, PCOS skin tags, or excessive hair growth on the body.
What does living with PCOS feel like?
Everyone’s experience living with PCOS is unique. Some people report irregular or skipped periods, others have painful or heavy periods. Some experience excessive hair growth on the body or face, hair loss on the scalp, sleep disturbances, mood swings, or changes in skin. No matter how PCOS manifests, it can impact your quality of life. Working with a PCOS specialist, such as the team at Allara Health, can help make symptoms more manageable.
How can I confirm if I have PCOS?
The only way to confirm if you have PCOS is to make an appointment with a PCOS specialist, such as an endocrinologist or gynecologist. They can assess your symptoms and order imaging and hormonal evaluations to determine if PCOS or something else is causing your symptoms.












