
Are Fibroids Causing Your Symptoms? Here’s How to Tell
That heavy bleeding, bloating, or pelvic pressure you can’t quite explain? It could be one of the common signs of fibroids. Knowing what to look for is the first step to getting answers and feeling better fast.
Signs of fibroids can be sneaky. Heavy periods, pelvic pressure, bloating. Are they just “normal period stuff” or something more? Odds are, you know someone with fibroids (or you have them yourself). In fact, up to 80 percent of people with a uterus will develop these benign muscular growths by the time they turn 50.
While I haven’t had fibroids personally, plenty of my friends and family have. Years ago, a colleague told me she had a fibroid so big it made her look pregnant—yes, that’s a thing, and I didn’t even know it was possible until she told me.
Like an enlarged belly (a.k.a. fibroid belly), there’s a whole menu of possible uterine fibroid symptoms, and they can be confusing. Just because fibroids are common doesn’t mean you should have to put up with frustrating or even debilitating side effects.
Ahead, we’ll walk through the most common signs and symptoms, how to tell if fibroids might be the culprit, and what you can do to get relief.
What are uterine fibroids?
Fibroids are muscular tumors that develop primarily in the uterus (aka womb). Also called uterine leiomyomas or myomas, these growths are almost always benign (non-cancerous) but can still cause some trouble for some people (more on possible symptoms later).
Fibroids can appear as a single lump or in multiples. Size-wise, they range from a tiny apple seed to a hefty grapefruit (and in rare cases, even larger). Somewhere between 20% and 80% of women develop fibroids by age 50, most often in their 40s and early 50s. That big range exists because many people with fibroids don’t have symptoms, so they may never know they have them.
African-American women face a higher risk of fibroids, and your odds climb even more if a family member has them, says ob-gyn Sherry Ross, MD, co-founder of Oneself Intimate Skin Care and author of She-ology and The She-quel.
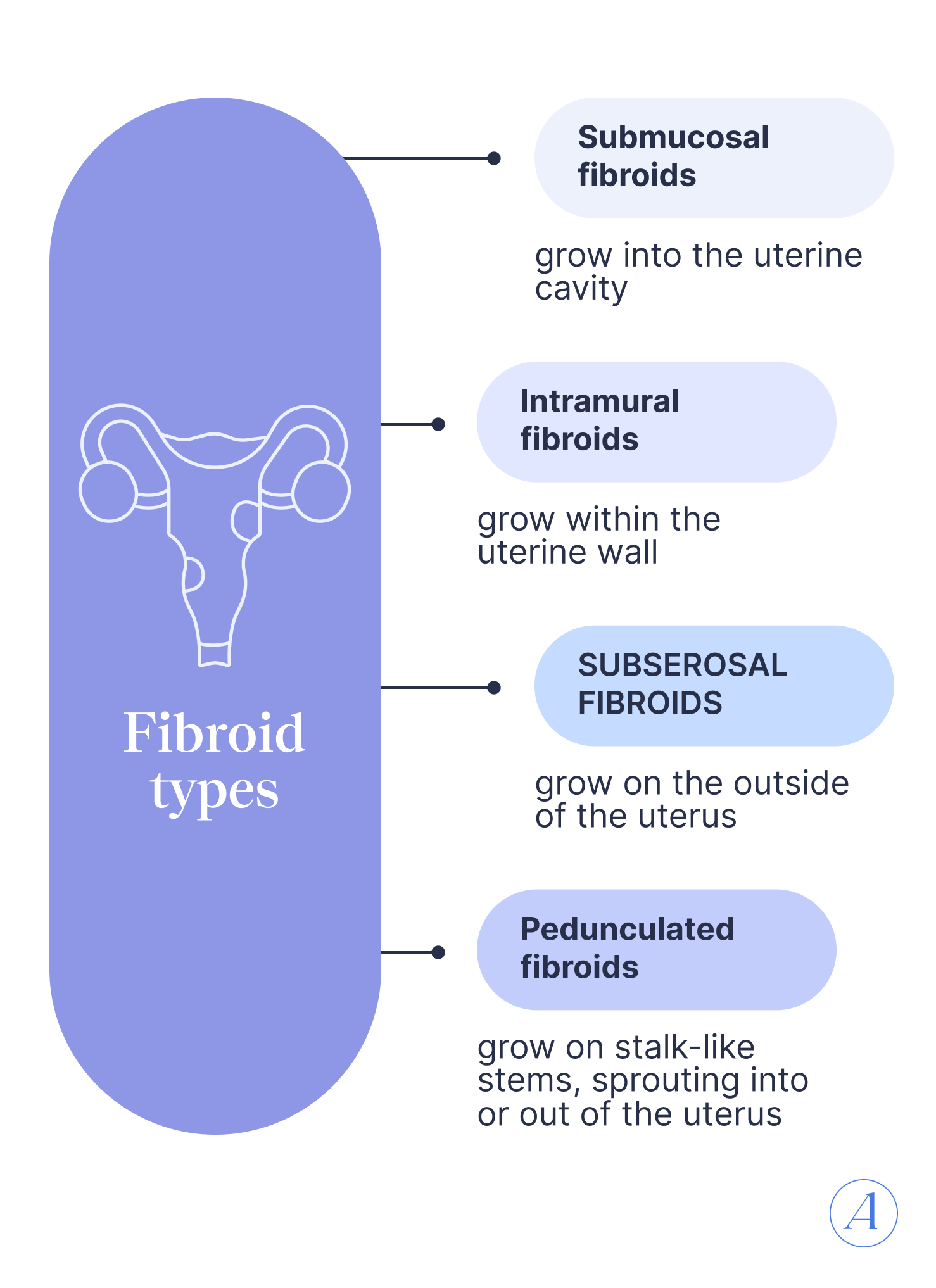
While most fibroids form in the uterine wall, they can grow in other places too. Doctors generally group fibroids into three main types depending on location:
- Submucosal fibroid – grow into the uterine cavity
- Intramural fibroid – grow within the uterine wall
- Subserosal fibroid – grow on the outside of the uterus
Some fibroids (pedunculated fibroids) grow on stalk-like stems, sprouting into or out of the uterus like mushrooms. Other fibroids are tiny “seedling” myomas (4 mm or smaller) or parasitic myomas, which latch onto other organs for a blood supply.
Subserosal and intramural types make up about 95% of fibroids, with submucosal fibroids making up the remaining 5%. But here’s the catch: fibroids rarely stick to one category. Many are hybrids (for example, a mostly intramural fibroid that also pushes into the uterine cavity). This overlap means classification is useful, but not always exact.
Diagram of fibroid types:
Submucosal fibroid – grow into the uterine cavity
Intramural fibroid – grow within the uterine wall
Subserosal fibroid – grow on the outside of the uterus
Pedunculated fibroids – grow on stalk-like stems, sprouting into or out of the uterus
Signs and symptoms of fibroids
Fibroids aren’t always troublemakers—many women don’t even know they have them. But when they do cause symptoms, they can seriously interfere with your life. Here’s what to watch for and why it’s worth getting help.
Heavy or prolonged bleeding
Heavy or drawn-out menstrual bleeding is one of the most common signs of fibroids, affecting 20% of or up to half of women who have them.
Fibroid-related bleeding usually happens during your period (known as menorrhagia or hypomenorrhea) and can be so heavy you’re may be changing pads or tampons every hour. This is especially common with submucosal fibroids, which grow inside the uterine cavity.
It’s not just inconvenient—excessive bleeding can lead to anemia, leaving you feeling wiped out, weak, and short of breath. But here’s an important side note: bleeding between periods isn’t usually caused by fibroids and should always be checked out by a doctor.
Pelvic pressure and fullness
A heavy, full sensation in your pelvis is another telltale sign of fibroids.
Fibroids can enlarge and distort the uterus, creating lumps and bumps that press on nearby organs. This can show up as a sensation of pressure, says Victoria Petruzzi, MD, an ob-gyn at Houston Methodist Willowbrook.
Depending on their location, fibroids can also squeeze the bladder (cue frequent bathroom trips) or press on the bowel (hello, constipation), Dr. Petruzzi says.
Lower belly swelling (“fibroid belly”)
When fibroids get big, they can make your belly look like you’re a few months pregnant even when you’re not.
Believe it or not, doctors often describe fibroid size the same way they describe pregnancy. For example, a “12-week-size fibroid uterus” means your uterus has expanded to the size it would be at three months pregnant. In some cases, it can grow to the size of a five-month pregnancy.
Pain or discomfort during sex
If sex hurts, it’s worth investigating. Some studies link fibroids—especially those at the top of the uterus (fundal fibroids)—to pain before, during, or after intercourse.
You don’t have to just “deal with it.” A trusted healthcare provider can help figure out if fibroids are to blame and offer treatments so intimacy is comfortable again.
Back, hip, or leg pain
When a fibroid grows big enough to “outgrow its space in the pelvis,” it can press on nearby organs, nerves, or joints, triggering pain in your back, hips, or legs, says Dr. Petruzzi.
Large fibroids at the back of the uterus can press on the lumbosacral plexus—a nerve hub that affects your lower back, hips, and legs—causing radiating discomfort, explains David Ghozland, MD, a gynecological surgeon. And if a fibroid gets really large (think 8 centimeters or more), its weight can throw off your posture and muscle balance, leading to nonstop aches in these areas, Dr. Ghozland adds.
Constipation or rectal pressure
If you’re backed up and can’t figure out why, fibroids could be part of the problem. Large fibroids can crowd nearby organs, including the bowel, creating rectal pressure and making it harder for things to move through smoothly. That pressure can lead to constipation, abdominal pain, or discomfort when you try to go.
Frequent urination or trouble emptying your bladder
Fibroids can mess with your bathroom habits in more than one way. While they can make pooping harder, fibroids can also make you pee more often by pressing on your bladder. For some people, that even means bladder leaks (a.k.a. incontinence).
In rare cases, fibroids can make it hard to empty your bladder at all. If a large fibroid squeezes a ureter (the tube that carries urine from a kidney to the bladder), it can block urine flow completely. When that happens, surgery is needed ASAP to prevent urine from backing up into the kidney, which can cause permanent damage.
Sharp, stabbing pain or burning sensation
Pedunculated fibroids—the ones that dangle from the womb on a thin stalk, kind of like mushrooms—can pack a painful punch. Quick or sudden movements can make them twist on that stalk, cutting off their own blood supply (a process called torsion). The result? Sharp, stabbing pain that can stop you in your tracks. You might also feel nauseous or spike a fever.
It’s not just pedunculated fibroids that hurt. Fibroids that grow quickly or start breaking down can also trigger intense pain.
Fertility and reproductive issues
Fibroids are behind roughly 5%–10% of infertility cases. Sometimes their location is the problem—a fibroid can block the fallopian tubes, making it harder for an embryo to implant or for assisted reproductive technologies to work. While research on fibroid-related fertility issues is limited, most experts agree that large fibroids or those that physically distort the shape of the uterus are more likely to cause problems. That’s why doctors may suggest checking the shape of your uterus if you are having difficulty conceiving.
The good news: Most women with fibroids can still get pregnant, and many have healthy pregnancies without complications. But size and location may matter. It is thought that multiple fibroids, large ones, or those in certain spots (like within the uterine wall or under the lining) can possibly raise the risk of miscarriage. And if a fibroid grows low in the womb, it might block the baby’s head from moving into position for birth.
If pregnancy is your goal, talk with your provider about your personal risks and what can be done to improve your chances.
What do fibroids feel like?
Fibroid pain runs the gamut from barely-there twinges to “can’t-get-out-of-bed” agony. How much it hurts depends on the size, number, and location of the fibroids. For some, it comes and goes. For others, it’s a constant companion. Many people notice the pain ramps up around their period.
No two people’s experiences are alike, but here’s how fibroid pain often makes itself known:
- Pressure and heaviness: Fibroids can enlarge the uterus, creating a heavy, full feeling in the pelvis, Dr. Petruzzi says.
- Worse menstrual cramps: As fibroids grow, they stretch the uterus, which can trigger bloating and more intense cramps during your period.
- Dull aches: Large fibroids can press on nerves, muscles, or pelvic structures, leading to achiness and stiffness in the back, hips, or legs, Dr. Ghozland says. They can even affect posture and muscle balance, adding to discomfort, he says.
- Sharp, sudden, or burning pain: Acute pain may be signs of fibroids breaking down. When a fibroid loses its blood supply and starts to break down (called degeneration), pain can spike suddenly, Dr. Ross says. Stabbing pain can also strike when pedunculated fibroids twist on their stalk, cutting off their own blood supply.
- Positional pain: Your pain might shift depending on how you move or sit, Dr. Ghozland says. In certain positions, large fibroids can press on specific organs or nerves, making discomfort worse.
Sometimes pinpointing the cause of the pain can be tricky since fibroid pain can overlap with other gynecologic conditions, including:
- Endometriosis
- Interstitial cystitis (painful bladder syndrome)
- Adenomyosis
- Pelvic inflammatory disease (PID)
- Ovarian cysts
To get to the bottom of your pain, your provider will piece together your symptoms using your health and period history, a pelvic exam, lab tests (like urine culture or STI screening), and imaging like a pelvic ultrasound, Dr. Ross says. This process helps pinpoint whether fibroids—or something else—are to blame. Getting the right diagnosis is the first step toward the right treatment and relief.
For example, it’s important not to conflate the symptoms of fibroids with the symptoms of, say, endometriosis. While these conditions can include some overlapping symptoms, such as heavy periods, they are very different diagnoses that require different treatment approaches. This is why consulting with a clinical expert is key.

Fibroids in perimenopause and after menopause
If you’ve dealt with fibroids in your reproductive years, things may change once you hit perimenopause or menopause, i.e., the time when your periods stop for good. That’s because hormones, especially estrogen and progesterone, play a big role in fibroid growth.
Fibroids tend to thrive when estrogen is high, says Dr. Ross. That’s why they can grow quickly during pregnancy. But once menopause hits and estrogen levels plummet, many fibroids shrink, she says. Sometimes this shift can ease symptoms.
That said, not all fibroids get the memo to quiet down. They “can still cause symptoms after menopause because they take up extra space in the pelvis, which can lead to chronic pelvic pressure, pain, or bladder and bowel issues,” explains Dr. Petruzzi. Dr. Ross adds that large fibroids can press on surrounding organs, tissue, or nerves, triggering discomfort even without high hormone levels.
Some people with fibroids even experience vaginal bleeding after menopause, which can be confusing if your periods have already stopped. But here’s the thing: postmenopausal bleeding is never considered normal. While fibroids can be the culprit, other causes include atrophy of the lower reproductive tract (responsible for about 60% of cases), infections, and even endometrial cancer (bleeding is present in about 90% of postmenopausal people with the disease).
If you notice any bleeding after menopause, don’t brush it off. See a healthcare provider promptly for a thorough evaluation to get to the root cause and the right treatment.
When to see a doctor (and what happens next)
Most women with fibroids never feel a thing. If yours aren’t causing symptoms, you may not need treatment. Your doctor will simply keep an eye on them during regular check-ups.
But if you are having symptoms, it’s time to speak up. Dr. Ross recommends seeing your provider if you have:
- Persistent irregular or heavy bleeding
- Painful periods
- Pelvic or lower back pain/pressure that interferes with life
- Ongoing urinary issues
- Chronic constipation
- Recurrent miscarriages
- Infertility
- Noticeable abdominal swelling
Some red flags that need urgent medical attention, according to Dr. Petruzzi, include:
- Severe anemia that might require a transfusion (often from heavy bleeding)
- An expanding belly close to the size of an early pregnancy
Your doctor might first suspect fibroids during a routine pelvic exam, feeling a lump or mass on your uterus. To confirm, they can use imaging tests such as:
- Ultrasound: Uses sound waves for a clear picture (done on the abdomen or inside the vagina)
- MRI: Uses magnets and radio waves for detailed images
- X-ray: Uses radiation to see inside the body
- CT scan: Takes multiple X-rays from different angles for a fuller image
- HSG or Sonohysterogram: Involves injecting dye or water into the uterus for X-ray or ultrasound imaging
If you’re diagnosed with fibroids, treatment is highly personal. Your plan depends on your symptoms, age, and whether you want children.
For mild symptoms:
- Over-the-counter pain relievers (ibuprofen, acetaminophen)
- Iron supplements for heavy-bleeding-related anemia
- Hormonal birth control (low-dose pills, progesterone injections like Depo-Provera, or a Mirena IUD) to manage bleeding
- Gonadotropin-releasing hormone agonists (injections, nasal sprays, or implants) to shrink fibroids
For moderate to severe symptoms:
- Myomectomy: Removes fibroids but leaves the uterus intact (best if you want to keep fertility)
- Hysterectomy: Removes the uterus (the only definitive cure)
- If fibroids are not too big, an endometrial ablation may be an option. This destroys the uterine lining to control heavy bleeding (no pregnancies possible afterward)
- Myolysis: Destroys fibroids with electric current or freezing
- Uterine Fibroid Embolization (UFE/UAE): Blocks blood supply to fibroids so they shrink
While this might seem like a lot, you don’t have to figure it out alone. Experts—like those at Allara—can guide you through diagnosis and treatment planning from the comfort of your own home, so you can start feeling better sooner.
A final word
Fibroids are incredibly common, but their impact is anything but one-size-fits-all. Some people may not even know they have them, while others deal with pain, pelvic pressure, urinary issues, or bleeding that interferes with daily life. Growth patterns depend on hormones, and symptoms often come down to where the fibroid is located rather than its size alone.
If you’re dealing with unexplained symptoms—or you’ve been told to “just live with” your fibroids—you have options. The experts at Allara can help you get answers, pinpoint the cause, and create a treatment plan tailored to your body so you can get back to feeling in control.
Key takeaways
- Fibroids affect everyone differently. Some people never have symptoms, while others face pain, pressure, heavy bleeding, or fertility issues that can seriously affect quality of life.
- Size and location matter. Large fibroids can press on organs, cause bloating, or, in rare cases, raise clot risk. Even small fibroids can cause major problems depending on where they grow.
- Hormones drive growth. Estrogen and progesterone levels can affect fibroid growth, especially during reproductive years and pregnancy.
- Heavy bleeding isn’t just annoying. It can lead to anemia, fatigue, and even require urgent care.
- Symptoms can shift with menopause. Fibroids often shrink after menopause, but they can still cause pain, pressure, or bladder issues.
- Fibroids are treatable. From medication to procedures, there’s a wide range of options to help manage symptoms and improve quality of life.
Frequently asked questions (FAQs)
Which size of fibroid is dangerous?
When it comes to fibroids, size isn’t the whole story—location is just as critical. A tiny fibroid in just the wrong spot can cause more havoc than a much bigger one somewhere less critical, Dr. Petruzzi says.
For example, a 2cm fibroid inside the uterine cavity can lead to disruptive bleeding while a larger 6cm fibroid on the top of the uterus might not cause any issues at all, Dr. Ross says.
In rarer cases, fibroids can press on major veins, increasing the risk of a blood clot, Dr. Petruzzi adds.
Bottom line: it’s less about “how big” and more about “where.”
What causes fibroids?
The short answer: no one knows for sure. But research points to a mix of factors, including:
- Genetics – If your mom had fibroids, your risk is about three times higher.
- Hormones – Estrogen and progesterone seem to impact fibroid growth.
What does a fibroid belly look like?
When fibroids grow large, they can give your belly a “pregnant” look even if you’re not expecting. Doctors often compare fibroid size to pregnancy: a “12-week-size fibroid uterus” means your uterus is about the size it would be at three months pregnant. In extreme cases, fibroids can stretch the uterus to the size of a five-month pregnancy.
Can fibroids cause anemia?
Yes—especially if they cause heavy or prolonged periods. That kind of bleeding can drain your iron levels, leading to anemia. In severe cases, anemia from fibroids may be bad enough to require a blood transfusion, Dr. Petruzzi says.
If you notice heavy bleeding, fatigue, or weakness, talk to your provider. They can create a treatment plan to manage fibroid symptoms, which might include iron supplements to help get your energy back on track.












