
Endometriosis statistics: what the numbers reveal about this common condition
Endometriosis statistics are all over the place. Some health insurance companies claim about 1% of people who menstruate have endometriosis, while clinical studies estimate it could be as high as 21%. While the stats vary greatly, they paint a story of the recent progress in understanding this medical condition and highlight how far we have to go in understanding this disease.
Anyone with endometriosis, a condition where cells similar to the lining of the uterus grow in other parts of the body, can tell you about how symptoms impact their lives. What’s less clear is how many people are affected by this condition and why it can take up to ten years to diagnose it.
While figuring out the exact prevalence and how to improve endometriosis treatment are best left to the medical experts, more awareness around this condition can help us all better understand the signs to look out for in ourselves and loved ones. To help, here’s the most up-to-date, comprehensive endometriosis statistics, including how many people are affected, the most common symptoms, and promising new diagnostic tools.
How common is endometriosis?
So just how common is endometriosis? That depends on who you ask. Health insurance companies estimate less than 1% of people who menstruate have endometriosis. If we’re looking at how many people self-report having endometriosis, the number rises to 6.8%, and prevalence based on symptoms observed by medical professionals is as high as 21%. Many official organizations, like the World Health Organization, place worldwide prevalence at around 5-10%.
Statistics on the lower end often don’t include transgender, gender-fluid, and nonbinary people, creating a gap in how we perceive the disease’s prevalence. A landmark 2024 study, for example, suggests the rate is as high as 25.14% among people who are transgender, nonbinary, and gender-fluid.
If we accept the more conservative estimate of 5%-10%, that means either one in twenty or one in ten people who are biologically female and of reproductive age (15-44) has this medical condition. Viewing prevalence as either one in ten or one in twenty emphasizes how large the potential range is. Regardless of the statistic, it is clear that endometriosis is often under-diagnosed or misdiagnosed.
Global prevalence
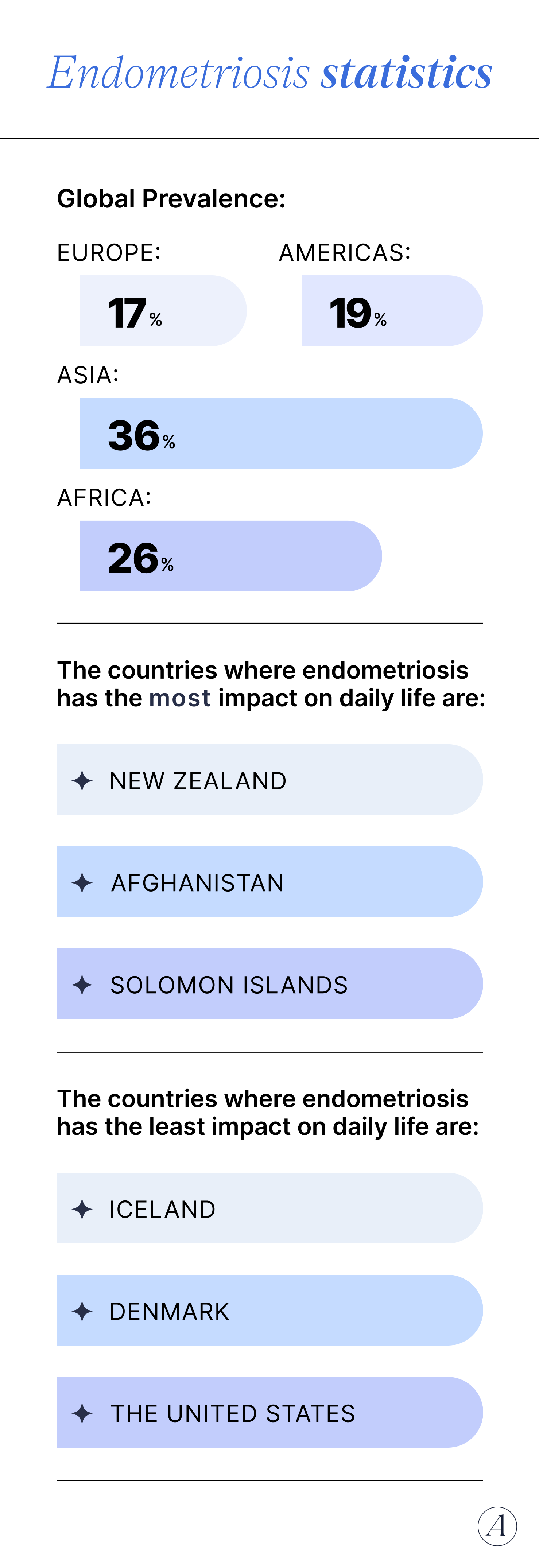
Endometriosis rates vary by continent:
- Europe: 17%
- Americas: 19%
- Asia: 36%
- Africa: 26%
It’s important to note that these statistics were pulled from a meta-review of select clinical trials which placed global prevalence at 18%, higher than other estimates.
As anyone with endometriosis will tell you, the condition isn’t just a simple yes/no diagnosis; its severity and impact on daily life vary greatly. The countries where endometriosis has the most impact on daily life are:
- New Zealand
- Afghanistan
- Solomon Island
The countries where endometriosis has the least impact on daily life, often due to comprehensive treatment and support, are:
- Iceland
- Denmark
- The United States
U.S. prevalence
Endometriosis prevalence in the United States was conservatively placed at 11% in 2011. More recent studies suggest prevalence could be as high as 15%, and an estimate from Illinois' state government places the prevalence between 10-20%. There hasn’t been any comprehensive data on how this rate differs by state, another gap in the story of endometriosis.
Endometriosis demographics
Endometriosis affects all kinds of people, but certain groups are more likely to receive a diagnosis.
Endometriosis prevalence by race
In the United States, endometriosis is more often diagnosed in white people than those of other races. This doesn’t necessarily mean it’s more prevalent, just that it’s more likely to be detected—often related to lack of healthcare access and racial biases. There are also racial differences in the time it takes to diagnose endometriosis (for the aforementioned reasons and others), but the current data is not able to reflect how long patients have symptoms of endometriosis before seeking care.
Here’s the breakdown of known diagnoses by race:
- 10.1% of Black people who menstruate have endometriosis
- 7.4% of Hispanic people
- 11.3% of Pacific Islanders/Asian people
- 17% of white people
Endometriosis by age
Most endometriosis cases are diagnosed when people are in their 30s or 40s. More specific age-related endometriosis stats include:
- Those 18-30 waited 0.49 years from time of consultation for a diagnosis
- Those 31-40 waited 3.1 years from time of consultation for a diagnosis
- Endometriosis affects 2-5% of postmenopausal people, significantly less than those in their reproductive years. The incidence of endometriosis is less in the postmenopausal population secondary to the decline of natural ovarian function.
Endometriosis diagnosis delays and misdiagnosis statistics
The endometriosis diagnosis rate is much lower than other medical conditions and 47% of people with the condition see five or more doctors before getting a diagnosis.
Why? The diagnosis is hard to make. “A definitive diagnosis of endometriosis can only be made surgically, usually via laparoscopy,” says Heather Huddleston, MD. Dr. Huddleston is Allara’s Chief Medical Advisor and a specialist in reproductive endocrinology and infertility at the University of San Francisco’s Center for Reproductive Health. Laparoscopy is a surgical procedure where a surgeon examines organs in the abdomen and pelvis, looking for endometriosis lesions. “This means that diagnoses are often delayed until symptoms are severe enough to justify surgery. This is beginning to change, however. “Increasingly, some imaging techniques such as MRI have been explored as a way to identify endometriosis without this level of intervention,” adds Huddleston.
On top of that, over 65% of people with endometriosis were originally misdiagnosed. “IBS, in particular, is one of the most common misdiagnoses that patients receive before an accurate diagnosis of endometriosis is made,” says Serin Seckin, MD, FACOG, a gynecologist at Generation Next Fertility, “This diagnostic uncertainty can be frustrating and emotionally draining for patients who are seeking answers and relief.”
Endometriosis, pregnancy, and infertility statistics
“Endometriosis is also linked to infertility, which can bring an additional layer of emotional stress, especially for those struggling to conceive or feeling uncertain about their future family building plans,” says Dr. Seckin. The condition’s impact on fertility and pregnancy outcomes depends on severity and if coexisting conditions exist, but it almost always makes family planning more emotionally challenging.
- In women with endometriosis, 50% experience female infertility.
- Couples with mild endometriosis have a 2-4.5% chance of conceiving in 30 days compared to 15-20% of couples without the disease
- However, IVF may help address fertility issues for people with endometriosis. Those with endometriosis can still have successful outcomes with IVF, barring removal of endometriomas that could impact ovarian reserve and therefore stimulation.
Once someone has conceived, endometriosis can also affect how the pregnancy goes:
- There’s a higher chance of premature birth
- Vaginal bleeding during pregnancy affects 80% of pregnant people with endometriosis
- Postpartum bleeding is 1.3 times more common in people with endometriosis
Endometriosis symptoms, quality of life, and mental health
“The most common symptoms are pelvic pain and menstrual cramps,” says Tara Scott, MD, an OB/GYN who specializes in hormone health. She mentions that gastrointestinal symptoms are also quite common.
Here’s what the numbers say about endometriosis symptoms:
- 20-25% of people with endometriosis have menstrual disorders, such as extreme pain during periods or irregular periods.
- Pelvic pain occurs in about 50-80% of women with endometriosis.
- Up to 53% of those with deep infiltrating endometriosis experience urinary symptoms, such as bladder pain, urgency, or hematuria (blood in urine). However the prevalence of bladder symptoms is only up to 12% in all types of endometriosis.
- Up to 90% experience gastrointestinal symptoms like bloating, constipation, or nausea.
- In one study, 55% of those with endometriosis reported having another chronic condition, such as an autoimmune disease or endocrine disorder.
Over 70% of those with endometriosis live with some degree of unresolved pain, which can take a toll on physical and mental health. “Endometriosis can impact nearly every part of daily life,” says Dr. Seckin, “It can affect personal relationships, work or school, and overall physical and emotional well-being.”
The stats back up how far-reaching endometriosis’ impact is:
- Someone is absent or less productive at school or work 10.8 hours on average per week due to endometriosis pain.
- 64% feel judged at work for endometriosis symptoms.
- 60% report having anxiety and/or depression.
- 70% of those with endometriosis report above average stress levels.
- 60-70% report sexual dysfunction or distress due to pain.
- 70.8% report trouble sleeping due to endometriosis.
- Those with endometriosis spend 3.5 times more money on healthcare costs.
- Days lost at work and reduced quality of work due to endometriosis results in almost $16,000 of annual income lost per person with endometriosis.
Endometriosis treatment statistics
While there is no cure for endometriosis, there are three common treatment strategies: pain management, hormone suppression, and surgery. A healthcare provider can assess which treatment option is right based on an individual’s symptoms and their severity, as well as if they’re interested in getting pregnant in the future.
Pain medications are the oldest treatment, often used as a first line-of-defense:
- Non-steroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, may help relieve chronic pelvic pain that is observed with endometriosis.
- 89% of participants in one US-based study took opioids to help manage pain, even though 78% of those with endometriosis experienced negative side effects from this drug class.
- GnRH agonists, a hormone-based medication, can reduce endometriosis symptoms in 80-90% of patients.
As the GnRH agonist stat suggests, hormonal treatment is often effective at relieving pain. For those not trying to get pregnant, birth control is often used.
- Combined estrogen-progesterone contraceptives or progestins are the first line of treatment to suppress the ovary and lead to regression of endometriosis. These options can relieve pain and help you regain quality of life.
- A progesterone-releasing IUD can decrease your amount of ectopic endometrial cells and help with pelvic pain.
- If these options don’t work for you, GnRH agonist therapy can help, but long-term use should be limited due to side effects (such as hot flashes and bone mineral density loss).
In more severe cases, surgery may be required. The most common surgery types are laparoscopy (used to diagnose disease and remove lesions) and laparotomy (removes growths and scar tissues). They are effective, though people do experience recurrences, sometimes requiring follow-up surgeries:
- In one small study, 84% of people stopped using pain medication after surgery.
- 42% of patients have undergone three or more surgeries.
- 40-50% experience a recurrence of endometrial lesions within five years.
The third most common surgery, a hysterectomy, removes the uterus. It is effective, but only recommended for those who don’t want to become pregnant in the future:
- 2% of patients required an additional surgery.
- 14.6% of people in the US who were assigned female at birth have undergone a hysterectomy (though not always for endometriosis).
Endometriosis mortality statistics
Endometriosis does not decrease life expectancy, but can increase the chances of developing certain conditions:
- The risk of ovarian cancer is 1.3% for all people who menstruate at birth. That number rises slightly to 1.8% for individuals with endometriosis.
- 20% of people with endometriosis have reported suicidal ideation, compared to 5.3% of the general population.
- Those with endometriosis are at a higher risk for ectopic pregnancy, which in rare cases could be fatal.
Despite these risks, one study looked at the all-cause mortality rate in people between the ages of 36 and 54 years old who identified as female. The data in this study showed that, for women with surgically confirmed endo, their midlife mortality rate was actually lower than their counterparts. However, that difference may be more related to a difference in lifestyle or increased medical attention in the cohort that has endometriosis—rather than the condition of endo itself.
Research, funding, and effect on public health
Only 5% of global research funding goes to gynecological health. And that percentage applies to all issues affecting people who menstruate, which includes endometriosis as well as menopause, fertility issues, PCOS, menstrual cramps, pregnancy complications, postpartum depression, and the list goes on.
For endometriosis specifically, here’s what funding and research looks like:
- The National Institute of Health devoted $28 million to endometriosis in 2024, which was down from the $29 million awarded in 2023 but more than the $15 million in 2015.
- Funding for endometriosis research translates to $2 per patient per year.
- Over 2,000 peer-reviewed articles on endometriosis are published annually, a number which has steadily risen since 2000.
Key takeaways
- Endometriosis affects somewhere between 1-21% of women, though it’s probably closer to 21% than 1% thanks to high rates of misdiagnosis and underdiagnosis.
- While IVF, emerging treatments, and an increase in peer-reviewed articles provide hope, there’s still a long way to go in understanding this medical condition’s impact, how to speed up the diagnostic timeline, and to make sure everyone gets the treatment they medically need.
- Allara Health is leading the way, offering a more comprehensive treatment for endometriosis. If you’re wondering if you have endometriosis or want to discover effective treatment options, you can get started with our team today.
Frequently Asked Questions (FAQs)
How common is endometriosis?
Conservative estimates claim somewhere between 5-10% of people who menstruate have endometriosis. Prevalence is probably higher since the condition is often undiagnosed or misdiagnosed.
How long does it take to get an endometriosis diagnosis?
It can take up to ten years to get an endometriosis diagnosis. On average, people see five or more doctors before being diagnosed with this condition.
How many women have PCOS and endometriosis?
Globally, 5-10% of people who menstruate have endometriosis. 6-13% have PCOS. Both are underdiagnosed, meaning the actual prevalence may be higher. Plus, you can have both PCOS and endometriosis together.
How common is infertility with endometriosis?
Infertility is a common symptom of endometriosis, affecting up to 50% of people with this condition. Many with endometriosis find IVF dramatically increases the likelihood of conceiving.













