
How to test for endometriosis: your complete guide to diagnosis
Endometriosis is a chronic condition that can be hard to diagnose. A thorough evaluation often includes a comprehensive medical history, pelvic exam, imaging tests, and laparoscopic surgery.
Endometriosis is a chronic inflammatory condition in which cells similar to the lining of the uterus grow in places they don’t belong.
The road to getting an endometriosis diagnosis can be long and challenging. Studies suggest it takes an average of five to eight years to get a diagnosis. This is in part because many people believe, or are told, that periods are supposed to be painful. Because most endometriosis symptoms flare or get worse during menstruation, people with endometriosis often spend years thinking their symptoms might be normal. Even after seeking care, it can take years to get a clinical diagnosis, as the symptoms of endometriosis often mimic other conditions. Endometriosis can also be hard to visualize and assess, making diagnosis even more difficult.
However, early detection and treatment are crucial for managing symptoms and preventing disease progression. Read on to learn how to test for endometriosis and the different ways healthcare providers may check for endometriosis.
How do doctors test for endometriosis?
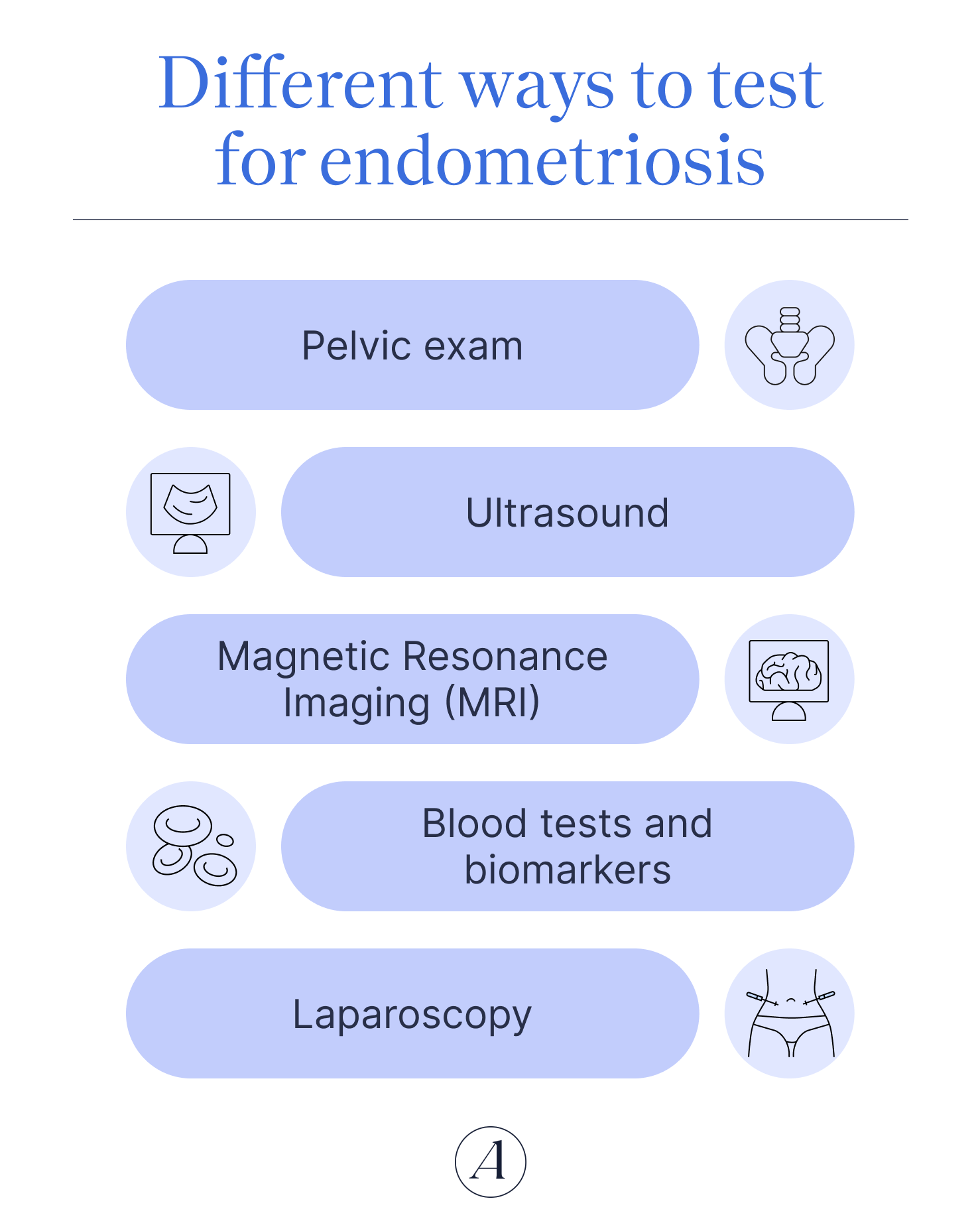
If your healthcare provider suspects you have endometriosis, they will likely recommend a series of tests in order to make a diagnosis. These tests may include a pelvic exam, ultrasound, MRI, and a laparoscopy. While the thought of undergoing these tests might be nervewracking, understanding what to expect can help alleviate some of the anxiety and uncertainty surrounding the diagnostic process.
Medical history and symptom review
Endometriosis can significantly affect your quality of life. The most common symptom of endometriosis that healthcare providers typically look for is period pain that disrupts your life and makes it difficult for you to engage in your regular activities. However, not everyone with endometriosis experiences such significant pain. Some people learn they have endometriosis after having difficulties getting pregnant.
Your healthcare provider will want to know what symptoms you’re experiencing and how long you’ve had them for as well as any family history of endometriosis, infertility, or chronic pelvic pain. Common symptoms of endometriosis include:

- Painful periods (dysmenorrhea): Periods that cause pain that disrupts daily life, making it hard to go to work, school, or engage in regular activities.
- Chronic pelvic pain: Pain that tends to be the worst during menstruation, but can, and often does, occur at other times in the cycle
- Pain during or after sexual intercourse (dyspareunia): Pain with penetrative sex as well as pain before, during, or after sexual activity
- Menstrual Irregularities: Heavy periods (menorrhagia), bleeding between periods, short or long menstrual cycles
- Infertility: Difficulty getting pregnant or a history of pregnancy loss
- Painful bowel movements or urination: Pain when using the bathroom may be due to endometrial-like cells on areas such as the bladder or colon. Other conditions common among people with endometriosis, like irritable bowel disease and interstitial cystitis, can also cause these symptoms
- Fatigue, bloating, and digestive issues: Endometriosis-related inflammation can cause other full-body symptoms even when the endometriosis lesions are limited to the pelvis
It's important to note that the intensity of these symptoms does not necessarily indicate the extent of the disease. “The interesting thing about endometriosis is that the symptoms of the condition do not always correspond to how much endometriosis is present,” says Gouri Pimputkar, DO, clinical lead at Allara Health. “You can have very few endometriosis spots seen on laparoscopy with very significant debilitating pelvic pain.“
Pelvic exam
After reviewing your symptoms, your healthcare provider will typically ask to do a pelvic exam. This exam allows them to feel, both internally and externally, for abnormalities in your pelvis, such as cysts or bands of scar-tissue called adhesions. Your abdomen may also appear distended and tender when touched.
A pelvic exam typically consists of two parts. First your healthcare provider will insert a speculum into your vagina to examine both the vagina and cervix. Then they will remove the speculum and manually examine the vagina with one or two gloved fingers. While they are doing this, they may press on your abdomen to better feel for any abnormalities as well as the position, shape, and size of your uterus and ovaries. In some cases, they may also insert a finger rectally and perform a rectovaginal exam.
Pelvic exams are often uncomfortable but they can be incredibly painful if you have vaginismus, a common condition among people with endometriosis, that causes the muscles in the vagina to involuntarily spasm. Let your healthcare provider know before the exam if you regularly have pain with penetration. They may be able to skip the speculum or use a smaller one, provide pain relief options, or skip the exam entirely. It’s important to communicate any pain or discomfort you feel during the exam. And don’t hesitate to let your healthcare provider know if you need to stop.
A pelvic exam alone cannot definitively diagnose endometriosis, but it can help identify areas of concern.
Ultrasound
An ultrasound is a non-invasive imaging test that uses high-frequency sound waves to create pictures of your internal organs. There are two types of ultrasounds that your healthcare provider may use to help diagnose endometriosis: a transvaginal ultrasound and a transabdominal ultrasound. During a transvaginal ultrasound, a small probe is inserted into your vagina to get a closer look at your reproductive organs. Transvaginal ultrasounds can help identify signs of ovarian endometriosis like endometriomas, a type of ovarian cyst associated with deep-infiltrating endometriosis.
A transabdominal ultrasound is an external scan that involves moving a probe over your abdomen. Ultrasounds cannot detect all forms of endometriosis, especially if the endometrial-like tissue is small or located in harder to scan areas.
Magnetic Resonance Imaging (MRI)
An MRI is a non-invasive imaging test that uses powerful magnets and radio waves to create detailed pictures of your anatomy. During the MRI, you'll lie on a table that slides into a large, tube-shaped machine. The test is painless, but some people feel claustrophobic inside the machine.
This test can provide more detailed images than an ultrasound and can detect deep-infiltrating endometriosis, nodular masses of endometriosis that can grow into organs and tissue, changing the way pelvic anatomy appears. A negative finding does not mean you don’t have endometriosis.
“Ultrasounds and MRIs are great at identifying endometriomas as well as deep endometriosis (better seen with MRI),” Pimputkar explains. “Neither imaging option is great at detecting superficial disease, which is the majority of what patients have.”
If you have any concerns about the MRI experience, talk to your healthcare provider beforehand. They may be able to recommend a facility that does open MRIs, which use less-tube like machines, or prescribe something to help manage your anxiety.
Blood tests and biomarkers
Your healthcare provider may recommend a blood test that measures CA-125 or cancer antigen 125. The test is typically used to monitor ovarian cancer progression, but a high result is not indicative of cancer. Menstruation, pregnancy, and endometriosis can all also cause higher levels of CA-125. And not everyone with endometriosis, especially younger people, has elevated levels. For this reason, experts don’t recommend using CA-125 as a diagnostic tool. However, your doctor may use it as part of a broader assessment combined with other imaging.
Professional recommendations also advise against measuring biomarkers in blood, menstrual or uterine fluids as a way of diagnosing endometriosis. These types of tests are an emerging area of science and currently cannot reliably diagnose the condition.
Laparoscopy
A laparoscopy with histological confirmation, taking tissue samples and looking at them under a microscope, is the most comprehensive way of diagnosing endometriosis. If you have signs of endometriosis on ultrasound or MRI, your healthcare provider may feel confident diagnosing you without laparoscopic surgery.
Laparoscopy is a minimally invasive surgical procedure performed under general anesthesia that allows the surgeon to visualize endometriosis lesions. Once you are asleep in the operating room, the surgeon makes a small incision near or inside of your bellybutton and inserts a thin, lighted tube with a camera on the end called a laparoscope. They will then make several more small incisions across your abdomen, so they can take tissue samples called biopsies. The biopsies then go to the lab to confirm the samples contain endometrial-like tissue.
Laparoscopic surgery can also treat endometriosis when it includes removing visible lesions. Oftentimes, surgeons skilled in diagnosing and treating endometriosis will remove any lesions and adhesions they see during the diagnostic laparoscopy, reducing the likelihood you’ll have to return for another procedure. It’s important to ask the surgeon performing your laparoscopy how often they diagnose and treat endometriosis, and if they plan on removing any tissue they suspect might be related to endometriosis.
How long the procedure takes depends on what the surgeon finds and how much scar and endometrial-like tissue they remove. Most laparoscopies last one to three hours but can be longer depending on how extensive the disease is. You will likely be able to go home the same day as the procedure. More complex cases may require an overnight hospital stay.
As with any surgical procedure, there are risks involved, such as infection, bleeding, and damage to abdominal organs and tissue. Your healthcare provider will discuss these risks with you and answer any questions you may have.
Why can it be difficult to get an endometriosis diagnosis?
Period pain isn’t normal, but many people think it is. Healthcare providers historically normalized period pain, especially in younger patients who were new to what menstruation felt like. Plus, endometriosis can run in families. So if you have an undiagnosed family member who grew up having painful periods, you might have been told that period pain is normal, since that’s all they knew.
“If you combine non-specific symptoms, lack of a definite test to diagnose, and an overall culture that normalizes pelvic pain, it can be easy to miss the diagnosis of endometriosis,” Pimputkar says.
You can get endometriosis regardless of your race or ethnicity. And you can have endometriosis regardless of your gender identity or sex. (Those with male anatomy can have endometriosis too, though it is rare.) But the medical field didn’t always recognize that endometriosis could occur across different age groups and races. This led to delayed diagnoses for many groups of people.
For a long time, endometriosis was thought of as a “career woman’s disease,” a condition found primarily in women who put off having children until later in their reproductive years. This way of thinking made it difficult for younger people to get a diagnosis, leaving many endometriosis cases undiagnosed and untreated.
Likewise, endometriosis was thought to only occur in white women. Instead of being diagnosed with endometriosis, Black women were frequently misdiagnosed with pelvic inflammatory disease. Though we now know these ways of thinking aren’t true, myths and biases about who gets endometriosis still exist.
Complicating matters further, endometriosis shares symptoms with a variety of other conditions. It can also co-occur with other health issues. This is part of what makes diagnosing endometriosis challenging. Depending on your symptoms, your healthcare provider may not suspect endometriosis at first.
Conditions that share symptoms with endometriosis include:
- Pelvic Inflammatory Disease (PID): PID is an infection of the reproductive organs that can cause pelvic pain and painful urination. PID may also be accompanied by fever, abnormal vaginal discharge, and a burning sensation during urination.
- Irritable bowel syndrome (IBS): IBS often causes diarrhea, constipation, or a combination of the two. It can also cause abdominal pain, painful bowel movements, chronic inflammation, and fatigue much like endometriosis. IBS is also more common in people with endometriosis.
- Ovarian cysts: Different from endometriomas, ovarian cysts can also cause period pain and abdominal bloating. Ovarian cysts can cause a dull ache or sharp pain in the lower abdomen, and the pain may come and go throughout the menstrual cycle.
- Fibromyalgia: Fibromyalgia is a chronic pain disorder that causes widespread pain throughout the body, including the pelvis, as well as fatigue. Fibromyalgia may also be also more common in people with endometriosis.
- Interstitial cystitis: Interstitial cystitis, also known as painful bladder syndrome, can cause chronic pelvic pain, pain during intercourse, and pain with urination, similar to endometriosis. Interstitial cystitis is also more common among those with endometriosis.
- Adenomyosis: Adenomyosis is a condition in which endometrial-like tissue grows into the muscular wall of the uterus, causing painful periods, infertility, and chronic pelvic pain. While adenomyosis and endometriosis often coexist, adenomyosis is confined to the uterus, whereas endometriosis occurs outside the uterus.
- Uterine Fibroids (leiomyomas): Uterine fibroids are non-cancerous growths in the uterus that can cause abnormal menstrual bleeding and pelvic pain. While fibroids and endometriosis can coexist, fibroids are more likely to cause heavy menstrual bleeding and pressure in the pelvis.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that affects the ovaries and menstrual cycle. PCOS can cause pelvic pain and irregular periods, symptoms associated with endometriosis, as well as unrelated symptoms like acne, excessive hair growth, and weight gain.
It's essential for healthcare providers to consider these and other conditions when evaluating a patient for endometriosis. By ruling out similar conditions, healthcare providers can better make a diagnosis and develop a personalized treatment plan to alleviate symptoms and improve quality of life.
What to do if your tests are ‘normal’ but symptoms aren’t
Though there are many tests that can indicate or suggest endometriosis, it’s still possible to have endometriosis even when tests appear normal.
“The tricky part about endometriosis is that there is no definite diagnostic test that can give a diagnosis for patients suffering from pelvic pain,” says Pimputkar. “Currently, the closest thing we have is a surgical procedure called a laparoscopy to identify and treat endometriosis. But, even with this invasive procedure, the diagnosis can sometimes be missed.”
You deserve comprehensive healthcare whether you have endometriosis or not. If your tests come back negative, don’t hesitate to get a second opinion. Endometriosis can be difficult to diagnose and not every healthcare provider is familiar with all of the ways endometriosis can present. Seek care with a provider who specializes in women’s health, knows what to look for, and will give you the whole-person care you deserve, like the experts at Allara.
Don’t give up investigating your symptoms. It's essential to establish an ongoing care plan with your healthcare provider to monitor your symptoms and adjust treatments as needed. Regular check-ups and open communication with your doctor can help ensure that your symptoms are being effectively managed.
The bottom line
Endometriosis can be a challenging condition to diagnose, but with the right support and resources, it’s possible to find the answers and care you need.
“The key for helping patients with suspected endometriosis is to validate their symptoms and listen to how the symptoms are impacting their lives,” says Pimputkar. “Depending on their goals, the treatment for endometriosis has to be individualized. There are instances where medical management is the preferred option and other times where surgical intervention may be needed.”
Key takeaways
- Diagnosis often takes years because symptoms are commonly normalized or overlap with other conditions and tests can miss endometriosis lesions.
- Imaging tests like ultrasounds and MRIs can detect deep-infiltrating endometriosis and endometriomas, a type of ovarian seen in people with endometriosis, but may miss superficial disease.
- Laparoscopy with biopsy is the most definitive way to diagnose endometriosis, and it can also be used to treat it.
- Normal test results don’t rule out endometriosis. Ongoing symptoms deserve further evaluation and care.
Frequently asked questions (FAQs)
Does endometriosis show up in blood tests?
Some people with endometriosis have elevated levels of CA-125 or cancer antigen 125. However, multiple conditions and health events, like pregnancy and menstruation, can cause elevated CA-125 levels and so experts don’t consider this test a reliable form of diagnosis.
How do I get a diagnosis for endometriosis?
There are several ways you can get an endometriosis diagnosis. A thorough endometriosis evaluation may include a comprehensive medical history, pelvic exam, ultrasounds, MRI, and laparoscopic surgery. If you have signs of endometriosis on imaging tests, your healthcare provider may be comfortable making the diagnosis without laparoscopy.
What are the red flag symptoms of endometriosis?
The hallmark symptom of endometriosis is period pain that disrupts your everyday life. If you can’t go to work or school when menstruating, you may have endometriosis. Consistently having to cancel plans or having difficulty doing daily tasks due to your period is not normal.
What age does endometriosis usually start?
Symptoms of endometriosis can start at any age. Many people with endometriosis start experiencing symptoms in their teens or when they start menstruating. Others may not have symptoms until their 20s or 30s, or when they start trying to have kids.











