Hormone testing for women: The essential guide to symptoms, testing, and next steps
Feeling “off” but your labs look fine? Hormone testing for women can help decode what’s really going on—just don’t expect a single blood draw to explain everything. We’ll walk you through what hormone tests can (and can’t) tell you, when to get tested, and how to get answers that actually make sense.
Hormone testing for women can feel like stepping into a funhouse of symptoms, theories, and lab reports—especially when your body is throwing curveballs faster than you can Google them. As someone with a chronic thyroid condition and a front-row seat to perimenopause, I know what it’s like. I’ve had stretches where my thyroid, estrogen, and progesterone labs look picture-perfect, and others where they’re doing cartwheels for no apparent reason. And without a provider who knows how to actually interpret those numbers—and treats me, not just the lab results—it can get rough, fast.
If you’re here, chances are you’re navigating your own “something feels off” era. Maybe your periods are acting unpredictable. Maybe you’re dealing with changes in your skin, hair, or mood. Maybe you’re exhausted, bloated, sweating at 2 a.m., or having trouble getting pregnant and wondering if it’s time to check hormone levels. Or maybe you’ve tried an at-home hormone test (or five) and still aren’t sure what any of it means.
You’re also probably sorting through a swirl of conflicting advice while trying to figure out when testing helps, when it doesn’t, and why your symptoms don’t always match your numbers. Here’s the truth: hormone testing is incredibly useful, but it isn’t magic. It’s a tool—an important one—but still only part of the story.
And that’s exactly what this guide is here to unpack. We’ll walk through common symptoms that indicate a hormone test may be beneficial, which hormones matter, how different testing methods work, what results can (and can’t) tell you, and how to take the next step toward getting the care you deserve. Let’s make sense of the noise, together.
When do you need hormone testing?
First things first: if you feel something is ‘off’ in your body, speak to your doctor immediately. You don’t need the perfect words or a neatly labeled symptom list; you know your body better than anyone, and that intuition is worth listening to.
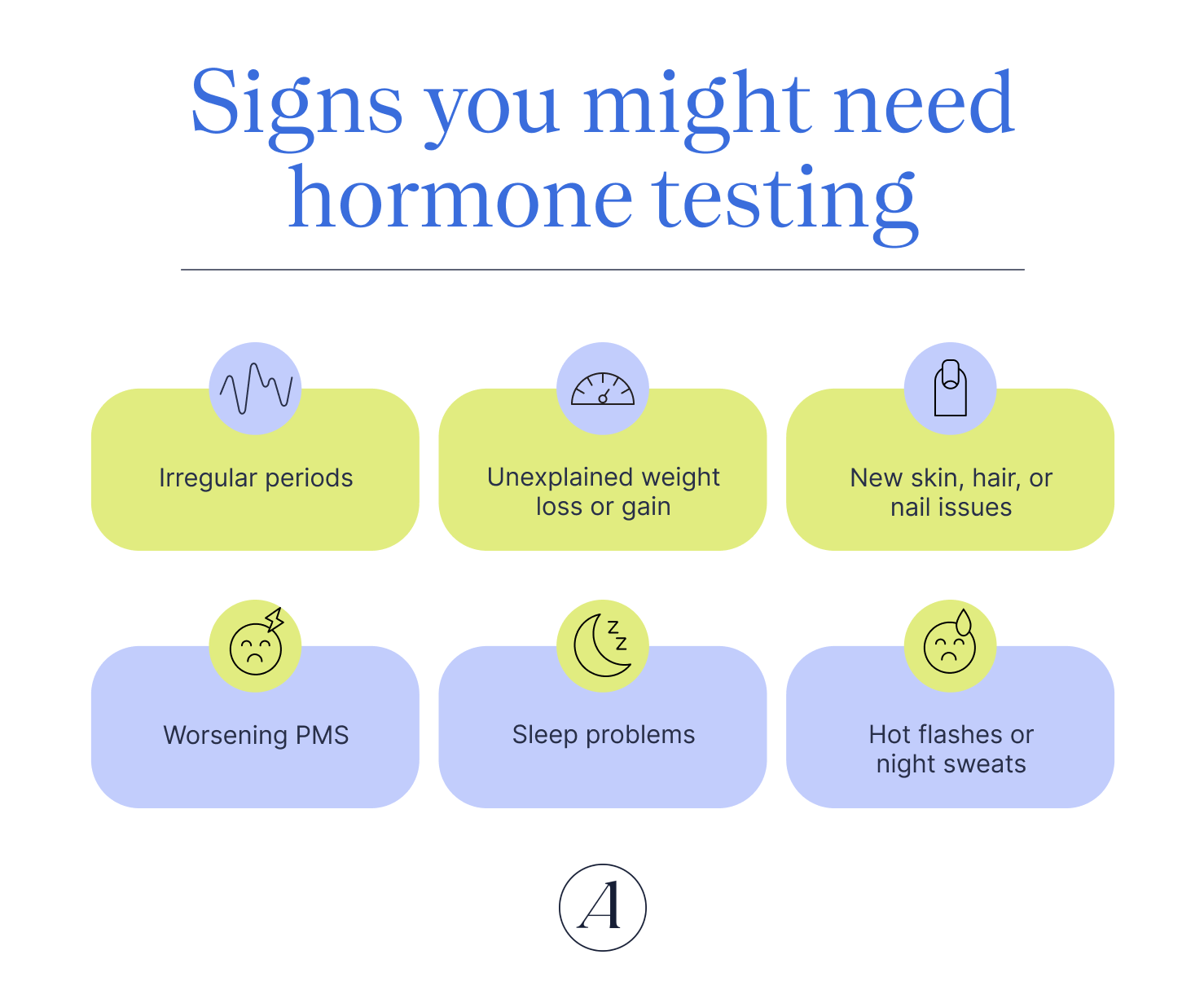
From there, you might also consider hormone testing, especially if you’re dealing with symptoms that just won’t quit. Hilary Booth, MS, RN, WHNP-BC, a women's health nurse practitioner at Allara Health, says common clues include:
- Irregular periods (timing between periods, length, spotting, or changes in flow)
- Unexplained weight loss or gain
- New skin (including acne), hair, or nail issues
- Worsening PMS
- Sleep problems
- Hot flashes or night sweats
Some symptoms, however, call for more urgent attention and prompt evaluation, says Booth:
- Soaking more than a pad an hour for four hours
- Passing clots larger than your palm
- Having thoughts of harming yourself or others
- Experiencing severe pain that doesn’t ease with basic measures like OTC meds or a heating pad
When it’s timed well and ordered for the right reasons, hormone testing can be incredibly helpful for getting to the bottom of symptoms like these. Still, it’s not always the right tool. Certain medications or supplements can artificially raise or lower hormone levels, making results harder to interpret, says Booth. That’s why it’s important to tell your clinician exactly what you’re taking before testing.
And timing truly matters. Hormones fluctuate throughout your cycle, so drawing blood at a random moment can lead to confusing or misleading results, says Booth. To get an accurate picture, testing usually needs to be done during specific windows—often in the first 2–5 days of your cycle, or sometimes after ovulation, depending on what your clinician is looking for, she explains. Plus, even with trying to time your hormonal testing in the right window, results can look normal—which can be frustrating. Just because a lab test is normal, does not exclude the diagnosis of perimenopause.
What are the different types of hormone tests for women?
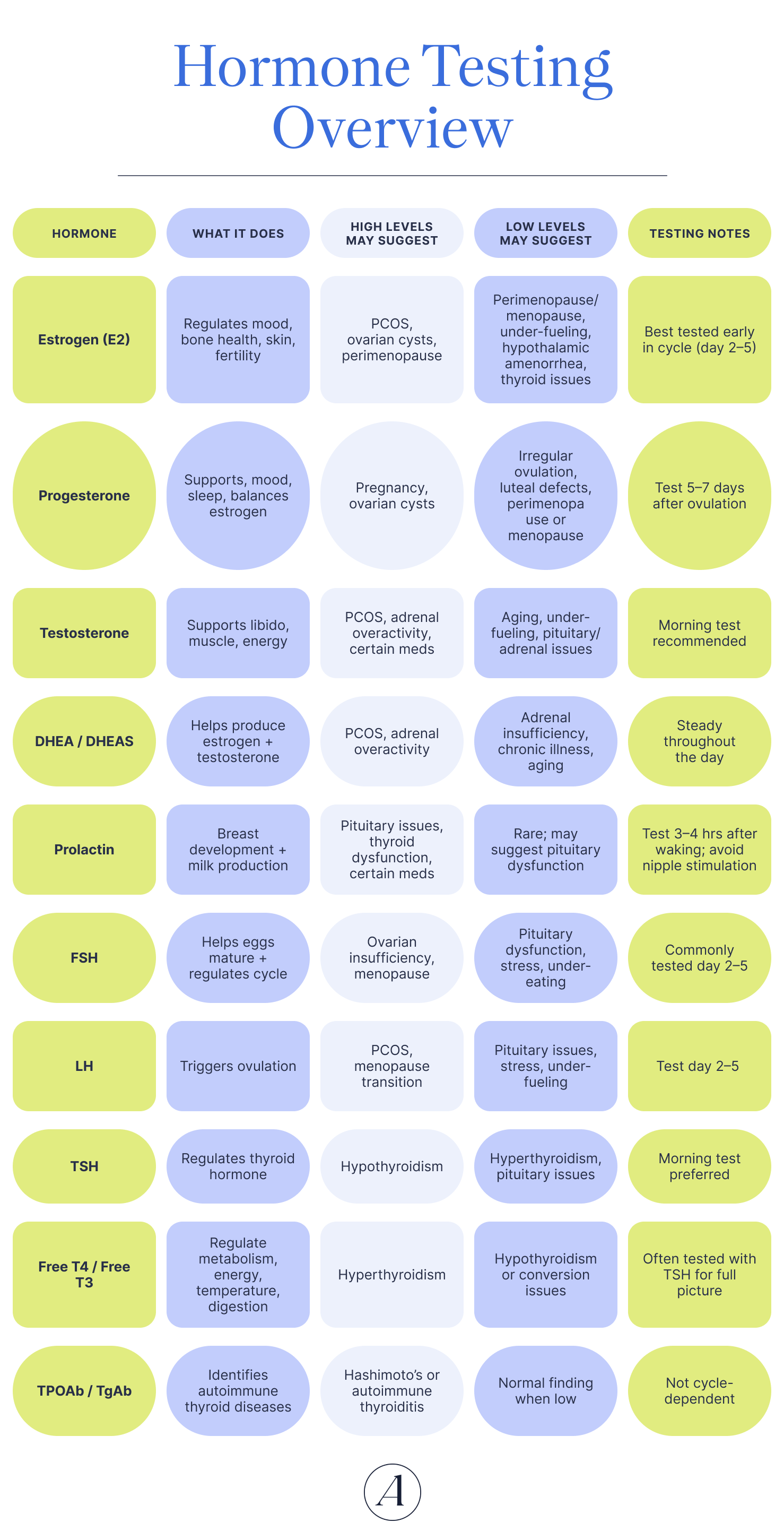
Curious what actually shows up on a hormone panel? There isn’t just one test—there are several, and each one tells a different part of your hormonal story.
Estrogen (estradiol, estrone, estriol)
Estrogen plays an essential role in puberty, periods, pregnancy, and menopause, but this hormone quietly keeps the rest of your body running, too. In addition to all its reproductive functions, it also helps regulate cholesterol and blood sugar, strengthens bones and muscles, and supports mood and cognition.
There are three types of estrogen:
- Estrone (E1)—the only type your body keeps making after menopause
- Estradiol (E2)—the main form produced during your reproductive years
- Estriol (E3)—peaks in pregnancy
These levels don’t stay still for long—estrogen rises and falls twice each menstrual cycle and shifts again across major life stages like puberty, pregnancy, and menopause.
But when estrogen stays consistently too high or too low, that’s when your body may be waving a red flag. You might need testing if you notice symptoms like:
- Early or delayed puberty
- Irregular or absent periods
- Trouble getting pregnant
- Symptoms of menopause
- Postmenopausal bleeding
- If you’re on hormone replacement therapy
Estriol testing can also play a role in monitoring high-risk pregnancies.
Because “normal” looks different depending on age and sex, results vary widely. Though for reference, typical estradiol blood test ranges are roughly:
- 30–400 pg/mL for premenopausal adults
- 0–30 pg/mL after menopause
Progesterone
Made from cholesterol in the ovaries and adrenal glands, progesterone earns its nickname—the “pregnancy hormone”—by prepping the uterine lining for implantation, calming uterine contractions to promote pregnancy, supporting gestation, and holding off milk production until after birth.
Mid-cycle, it helps grow new capillaries so your uterine lining gets the blood and nutrients it needs. It also thickens cervical mucus to keep harmful microbes (and sperm, at certain points) from slipping through.
After ovulation, levels rise, peak for about a week, then fall again if no fertilization happens. During pregnancy, though, progesterone keeps climbing steadily to support the developing fetus.
When progesterone swings up and down, that’s normal. When it stays too high or too low, that’s when symptoms can show up. Higher-than-expected levels typically reflect ovulation or pregnancy, but they can also overlap with premenstrual dysphoric disorder (PMDD) symptoms like irritability, mood swings, anxiety, and depression. In rare cases, very high levels can signal adrenal or ovarian tumors or congenital adrenal hyperplasia.
Lower-than-normal progesterone tells a different story. Low progesterone levels can be linked to amenorrhea (from not ovulating), irregular periods, ectopic pregnancy, miscarriage, or fetal death.
To give you a sense of the range, typical levels look roughly like this:
- Pre-ovulation: < 1 ng/mL (3.18 nmol/L)
- Mid-cycle: 5–20 ng/mL (15.90–63.60 nmol/L)
- Pregnancy, 1st trimester: 11.2–90.0 ng/mL (35.62–286.20 nmol/L)
- Pregnancy, 2nd trimester: 25.6–89.4 ng/mL (81.41–284.29 nmol/L)
- Pregnancy, 3rd trimester: 48–150+ ng/mL (152.64–477+ nmol/L)
- Postmenopausal adults: < 1 ng/mL (3.18 nmol/L)
Because progesterone fluctuates throughout the month and even day-to-day, a single test can miss the bigger picture, so your provider may track your levels more than once.
Luteinizing hormone (LH)
Luteinizing hormone (LH) is made in the pituitary gland and plays a starring role in your menstrual cycle, triggering ovulation. LH levels spike just before an egg is released, which is why many people track it when trying to conceive. If you’ve been struggling to get pregnant for 12 months, you’re lactating (when not pregnant or nursing), or your cycles have gone irregular or MIA, an LH test can help pinpoint what’s going on, from ovulation timing to potential causes of infertility.
Because LH naturally rises and falls throughout the month, context matters. When levels stay consistently high (outside of that pre-ovulation surge), it can signal an issue with how the ovaries are functioning. Conditions associated with elevated LH include:
- Primary ovarian insufficiency
- Polycystic ovary syndrome (PCOS)
- Adrenal or thyroid disorders
- Chromosomal conditions like Turner syndrome
High LH outside your ovulatory window may also indicate menopause.
On the flip side, low LH may point to a pituitary or hypothalamic issue or reflect external stressors like under-nutrition, significant weight loss, or chronic stress that disrupt hormone production.
For reference, LH ranges shift across the cycle:
- Follicular phase: 1.68–15 IU/mL
- Mid-cycle peak: 21.9–56.6 IU/mL
- Luteal phase: 0.61–16.3 IU/mL
- Postmenopause: 14.2–52.3 IU/mL
Follicle stimulating hormone (FSH)
Follicle-stimulating hormone (FSH), also made by the pituitary, works hand-in-hand with LH. Its main job? Helping follicles (aka the little sacs that house developing eggs) mature so ovulation can happen. You might need an FSH test if you’re experiencing abnormal vaginal or menstrual bleeding, trouble conceiving, or infe rtility.
While FSH naturally fluctuates as your cycle moves from follicular phase to ovulation, high levels often flag that the ovaries aren’t making sex hormones effectively, or that something outside the ovaries is affecting how the reproductive system functions. Common culprits mirror those linked to high LH: primary ovarian insufficiency, PCOS, thyroid or adrenal disorders, certain ovarian tumors, and chromosomal conditions like Turner syndrome. Menopause or perimenopause can also drive FSH up.
Lower-than-normal FSH typically points to a pituitary or hypothalamus issue, and—similar to LH—can also reflect extreme exercise, rapid weight loss, or being significantly underweight.
Here’s how typical FSH levels stack up:
- Before puberty: 0–4.0 mIU/mL
- During puberty: 0.3–10.0 mIU/mL
- Menstruating adults: 4.7–21.5 mIU/mL
- After menopause: 25.8–134.8 mIU/mL
Anti-mullerian hormone (AMH)
AMH—short for anti-müllerian hormone—is one of the most useful markers for understanding your ovarian reserve (aka how many potential egg cells you’ve got left). It can help explain fertility challenges and give you a sense of your overall reproductive timeline. Generally, higher AMH suggests more time to get pregnant, while lower levels may mean you shouldn’t wait too long if pregnancy is a goal.
But here’s the catch: AMH can’t tell you whether your eggs are healthy or predict whether you will get pregnant. It’s one piece of a bigger puzzle. It also has diagnostic value beyond fertility—higher levels can point to PCOS while very low levels may signal that menopause is approaching.
AMH naturally changes with age, rising in adolescence, peaking around 25, then steadily declining. Typical ranges include:
- Average: 1.0–3.0 ng/mL
- Low: Under 1.0 ng/mL
- Severely low: Around 0.4 ng/mL
No matter where your number lands, AMH results should always be interpreted with your primary care provider—and, if fertility is a concern, a specialist—who can put your results into proper context.
Testosterone (Total, Free)
Testosterone isn’t just a “male hormone”—people AFAB have (and need) it too.
In people AFAB, testosterone supports sex drive, muscle mass, and bone health. The hormone circulates in two forms: free testosterone (ready for your body to use) and bound testosterone (attached to proteins). Most testosterone is bound, and that’s a good thing. It prevents your body from using too much at once.
Providers typically measure testosterone through:
- Total testosterone, which includes both bound and free testosterone (most common)
- Free testosterone, the unbound portion (less common, but helpful in specific cases)
Testing is usually prompted by symptoms of excess or deficiency. In people AFAB, high testosterone can show up as facial or body hair growth, androgenic hair loss (hair thinning at the crown or temples), a deeper voice, or hormonal acne. Causes may include:
- PCOS
- Ovarian tumors or dysfunction
- Adrenal disorders like CAH
- Pituitary gland disorders
Low testosterone is normal in women, but extremely low levels may point to:
- Adrenal disorders
- Pituitary issues
- Ovarian dysfunction
For reference, typical total testosterone ranges for people AFAB are 15–70 ng/dL (0.5–2.4 nmol/L). And timing of testosterone testing is key: the most accurate results come from a morning blood draw between 7–10 a.m., when testosterone levels peak.
DHEA
Think of DHEA (dehydroepiandrosterone sulfate) as one of your body’s hormone building blocks—it’s the raw material your system uses to make estrogen and testosterone.
DHEAS plays a big role in puberty, reproduction, and overall hormonal balance. Levels peak in your teen years, then naturally drift downward with age.
When DHEAS levels are high, it often shows up in people AFAB as symptoms similar to elevated testosterone, including:
- Excess facial or body hair
- A deeper voice
- Irregular periods
- Acne
- Increased muscle mass
- Thinning hair at the crown
When DHEAS levels are low, it usually stems from an adrenal issue, or it can simply be age-related.
Typical DHEAS ranges for people AFAB vary by age:
- 18–29: 45–320 µg/dL
- 30–39: 40–325 µg/d
- 40–49: 25–220 µg/dL
- 50–59: 15–170 µg/dL
- 60+: <145 µg/dL
Prolactin
Meet prolactin: the hormone that helps grow breast tissue during pregnancy and kick-starts milk production after birth.
Because of that role, prolactin levels are expected to be high in pregnant or breastfeeding people and low in everyone else. When prolactin is higher than it should be outside of pregnancy, it can spark symptoms in women such as:
- Irregular or missing periods
- Milk production when you’re not breastfeeding
- Nipple discharge
- Difficulty getting pregnant
Low prolactin is much less common, but when it happens, it may signal a pituitary gland problem.
Typical prolactin ranges include:
- Nonpregnant people: <25 ng/mL
- Pregnant people: <500 ng/mL
Prolactin levels naturally rise and fall throughout the day, so most providers schedule the blood draw about 3–4 hours after you wake up to get the most accurate reading.
Thyroid Hormones (TSH, T4, T3, TPO, TPOAb)
Your thyroid—the tiny-but-mighty, butterfly-shaped gland at the base of your neck—helps set the pace for your metabolism, energy, mood, heart rate, and body temp.
To keep all that running smoothly, several key hormones work together:
- TSH (thyroid-stimulating hormone): Released by your pituitary gland, TSH is basically your thyroid’s manager, telling it when to ramp up or dial down hormone production.
- T4 (thyroxine): The main hormone your thyroid makes.
- Free T4: The active, ready-to-use form that travels to your tissues.
- Bound T4: Attached to proteins so it stays circulating as backup fuel.
- T3 (triiodothyronine): The hormone that actually does the work of driving your metabolism.
- Free T3: Ready to act.
- Bound T3: Stored and waiting, tied up to proteins; most of your T3 lives here.
Because T3 and T4 regulate how your body uses energy, even small dips or spikes can show up as big symptoms—think shifts in weight, mood, fatigue, anxiety, or and even how hot or cold you feel. That’s why your provider may order thyroid labs when something feels “off.”
They may also check for thyroid antibodies—TPOAb (thyroid peroxidase antibodies) and TgAb (thyroglobulin antibodies). Elevated levels can point to autoimmune causes like Hashimoto’s disease, where the thyroid struggles to produce enough hormone.
For reference, typical TSH values fall around 0.5 to 5.0 mIU/L, but there are exceptions. During pregnancy, after thyroid cancer, with pituitary conditions, or in older adults, optimal TSH targets can shift, and that’s where an endocrinologist guides the exact range for you.
Other hormones
Depending on your symptoms, your provider may want to test a few additional hormones to get the full picture. These aren’t always the headliners of reproductive health, but they absolutely influence how you feel day to day.
Cortisol
Made in the adrenal glands, cortisol helps you respond to stress, keep inflammation in check, regulate blood sugar and metabolism, and maintain blood pressure. When cortisol is out of balance—too high in conditions like Cushing’s syndrome or too low in Addison disease and adrenal insufficiency—you can feel it. A cortisol test helps sort out whether your symptoms line up with one of these conditions. Note, though, that both Cushing's and Addison Disease are rare. If there is suspicion that you have one of these conditions, work with an endocrinologist for specific testing that can more accurately measure your cortisol levels.
Insulin
Produced by the pancreas, insulin ushers glucose from your bloodstream into your cells so they can actually use it for energy. Testing insulin can help explain low blood sugar episodes, diagnose insulin resistance, and guide treatment for type 2 diabetes. If you’re dealing with shakiness, dizziness, or unexplained fatigue, this hormone may be part of the puzzle.
Growth hormone
Also called human growth hormone (GH), it fuels growth and keeps your metabolism humming. In kids, GH is essential for height, bone growth, and muscle development. In adults, it maintains bone strength and muscle mass. Too little GH can lead to low bone density and muscle loss, while too much can cause conditions such as gigantism in children or acromegaly in adults—both marked by enlarged hands, feet, and facial features.
Melatonin
Produced mostly by the pineal gland, melatonin helps regulate your circadian rhythm—your natural sleep-wake cycle. If you’re tossing and turning or can’t fall asleep, testing melatonin can help identify sleep-related disruptions.
Serotonin
Though known for its mood-boosting reputation, serotonin regulates everything from behavior and memory to digestion. Serotonin testing isn’t routine; it’s mainly used when a provider suspects carcinoid syndrome, a condition caused by rare tumors that often drive serotonin levels abnormally high.
Leptin
Released by body fat, leptin helps regulate weight over time by signaling when you’ve had enough to eat. High leptin levels (hyperleptinemia) are linked to obesity and sometimes food-related compulsive behaviors.
Ghrelin
Made in the stomach, ghrelin—aka the “hunger hormone”—rises between meals to nudge your brain toward hunger and drops once you’re full. People with obesity often have lower ghrelin levels, whereas those who severely restrict calories tend to have elevated levels.
How does hormone testing work?
So your provider wants to check your hormones—now what? A hormonal imbalance test sounds intimidating, but the process is pretty straightforward. Depending on what your provider is looking for, hormones can be measured through blood, urine, or saliva. Estrogen, for example, can be tested using any of the three.
If you’re testing at a clinic or lab, you’ll typically give a blood or urine sample. A standard blood draw is the most common. A 24-hour urine test—sometimes used for an estrogen test—means collecting all your urine for a full day using a special container and specific instructions. At-home estrogen tests usually rely on saliva instead.
Some other hormones also lend themselves to at-home kits, like progesterone testing. PDG urine strips, which measure a progesterone metabolite, can offer useful clues, but they’re not perfect. Many hormone tests require very specific timing in your cycle, some work better when collected as saliva rather than urine, and shipping or storage issues can throw off results, says Booth. It’s “hard to guarantee that” the sample “will be transported correctly, which can lead to false positive or negative tests,” she explains.
Because of that, at-home hormonal tests are usually best seen as a starting point rather than the final word. Booth often recommends these kits for people who can’t easily get to a lab, feel anxious about blood draws, or simply want a baseline. But if anything looks unusual, it’s important to follow up with a provider who may repeat the test at a trusted lab, she adds.
Timing also plays a huge role in getting accurate results. Some hormones—like testosterone and prolactin—are best checked in the morning, and certain tests require fasting beforehand. If you have a menstrual cycle, the timing becomes even more important: many hormone levels fluctuate predictably throughout the month, so providers often target testing to days 2–5 of the cycle or post-ovulation depending on the clinical question, says Booth.
Before testing, you may also need to pause certain medications or supplements—such as hormonal birth control, hormone replacement therapy, or even biotin supplementation—because they can skew certain hormone levels like estrogen. Just make sure to clear any changes with your provider rather than stopping anything on your own.
Once everything is done, the good news is that results usually come back fairly quickly. Most labs return results within about a week, depending on the type of sample and testing method.
What hormone tests can (and can’t) tell you
Hormone tests can give you answers—but not every answer. While these labs can help diagnose or monitor certain conditions, they also have limits. In other words: don’t expect a single test to suddenly “explain everything.”
The main issue? Hormones are incredibly complex. They operate through feedback loops, with glands constantly communicating, says Booth. Because these signals shift throughout the day—and definitely throughout the menstrual cycle—your results can vary depending on when the test is done.
And one snapshot rarely captures the whole movie. “Because a lot of hormone testing is a snapshot, it may not reflect what is going on all the time,” says Booth. Even a 24-hour urine collection won’t show hour-by-hour changes. This is why your provider may order multiple hormone blood tests to identify patterns instead of basing decisions on a single moment in time.
Subjective symptoms add another wrinkle. “A lot of how we feel is also subjective,” Booth says. Some people feel every tiny hormonal dip; others glide through major fluctuations without a blip. So labs matter, but they never tell the full story on their own.
This is especially true in perimenopause and menopause. Hormone levels during the transition can swing wildly for years, but these numbers don’t predict how intense symptoms will be, how long they’ll last, or when menopause will officially start. Diagnosis is usually based on age, symptoms, and not having a period for 12 months, not a single lab value, says Booth. Still, checking hormones can sometimes help rule out other conditions that mimic menopausal symptoms, she adds.
And then there’s the lab technology itself—another source of variation. Different manufacturers use different assay kits, which don’t always behave the same way or give identical results. Immunoassays, a common testing method, can also be nonspecific and prone to interference.
Bottom line: Hormone tests are incredibly useful tools, but they aren’t crystal balls. The real magic comes from pairing your lab results with your symptoms, history, timing, and a provider who knows how to interpret everything in context.
What to do if your results don’t give clear answers
When your labs don’t match how you feel, it can make you want to scream into a pillow. It’s confusing, it’s frustrating, and it can make you doubt your own experience. But don’t. “Continue to advocate for yourself,” says Booth. “You live in your body every day—we don't.”
Remember: one blood test is just a quick snapshot, not the whole picture. Labs can’t always capture the shifts and subtleties driving your symptoms. So even when your hormone levels fall in the so-called “normal” range, that doesn’t mean there’s nothing you can do to “help optimize and improve hormone function”—or that nothing is actually happening, says Booth.
This is where a good provider makes all the difference. It’s important to have someone who “can interpret the tests and listen to your symptoms,” Booth says. That’s how you get an individualized plan that actually supports your hormone health, whether that’s medication, supplements, lifestyle changes, or a combination, she says.
How Allara approaches hormone testing
At Allara, the goal is simple: understand what’s really going on in your body. The approach starts with comprehensive testing—not just hormones in isolation, but how your endocrine, gynecologic, and metabolic systems interact.
From there, providers build a plan that treats you like a whole human, not a lab result. That might include vitamins, supplements, meal planning, movement, stress and sleep strategies, social support, and medication when needed. It’s all designed to work together, not in silos.
And the support doesn’t end after the first appointment. Allara providers track your progress throughout your membership with follow-up labs and regular check-ins to adjust your plan as your body changes.
Even if your labs come back “normal,” you won’t get brushed off. Allara’s clinical team reviews results with you, listens to your symptoms and concerns, and works collaboratively to figure out what’s next—diagnosis or not. The goal is to make sure you’re actually getting the care you need, not just the care your numbers suggest.
The bottom line
Hormone testing can be incredibly helpful, but it’s not perfect. Because hormones work in complex loops and shift constantly, labs capture only a brief moment in a much bigger pattern. That’s why results don’t always line up with how you feel, and why getting the right tests at the right time (plus a provider who actually listens) matters so much.
If your symptoms are still screaming even when your labs look “normal,” don’t write yourself off. Your lived experience matters, and with the right support, there are ways to optimize hormone function so your body finally feels like it’s working with you, not against you.
Ready to get real answers? The experts at Allara will investigate, diagnose, and build a personalized treatment plan so you can get to the bottom of your symptoms and feel in sync with your body again.
Key takeaways
- Hormone testing can help uncover the root of symptoms like irregular periods, weight changes, mood shifts, sleep issues, and hot flashes—but one test rarely tells the whole story.
- Hormone levels naturally fluctuate throughout the day and month, so timing matters; many tests need to be done during specific cycle days or in the morning.
- At-home tests can be convenient, but they’re less reliable than lab tests and often need follow-up with a provider.
- “Normal” labs don’t rule out hormonal issues—symptoms still matter, and interpretation requires context.
- Even with normal results, a skilled provider can help optimize hormone function through medications, supplements, nutrition, and lifestyle changes.
Frequently asked questions (FAQs)
When should a woman get her hormones checked?
If your body feels out of sync, hormone testing can help you figure out what’s up. According to Booth, common red flags include:
- Irregular periods (timing, length, spotting, flow changes)
- Unexplained weight loss or gain
- New skin, hair, or nail issues
- Worsening PMS
- Sleep problems
- Hot flashes or night sweats
If something feels off, trust that instinct and loop in your doctor. No one knows your body better than you do.
Can you ask your doctor for a full hormone panel?
Absolutely—you can and you should request a comprehensive hormone panel if something doesn’t feel right. Your symptoms are your best evidence, so come prepared with what you’re experiencing. That helps your provider decide which hormones actually need checking instead of running a generic (and often unhelpful) panel.
And if your provider dismisses your concerns? You’re allowed to find one who listens. Advocacy is part of good care.
When is the best time to test for hormone imbalance?
Timing is everything with hormones. Because levels rise and fall throughout your cycle, testing at a random moment can lead to confusing or misleading results, says Booth. That’s why clinicians usually target specific windows—often days 2–5 of your cycle or after ovulation, depending on what they’re evaluating, she says.
Time of day can matter, too. Some hormones—like testosterone and prolactin—are best checked in the morning. Your provider will guide you on the exact timing so you get the clearest, most accurate picture.












