
Understanding Addison’s disease: Symptoms and early signs
Low cortisol symptoms can go unnoticed, but signs like unexplained fatigue, hair loss, hyperpigmentation, and salt cravings could point to Addison’s disease.
Conversational Takeaway: By now, we’ve probably all seen the “cortisol detox” trend on social media. But what happens when cortisol levels are too low? Enter: Addison’s disease. This condition occurs when certain hormones, including cortisol, are low. It’s a difficult to diagnose condition because Addison’s disease symptoms are similar to many other conditions. Here’s how to tell if symptoms like fatigue, salt cravings, and dizziness stem from Addison’s disease or something else.
Addison’s disease occurs when adrenal glands, small glands that sit above the kidneys, don’t produce enough cortisol and aldosterone, two essential hormones. This condition is rare, with one estimate that it affects one out of every 100,000 people, though it’s most likely underdiagnosed, because Addison’s disease symptoms tend to manifest gradually and are nonspecific, meaning they’re similar to symptoms of other conditions.
Hilary Hodge, a patient with Addison’s disease and an advocate for parents with chronic illnesses, didn’t know she had this condition until she had an adrenal crisis—which we’ll get into a bit later. Since then, she’s been diagnosed with Addison’s disease, started on a treatment plan to manage symptoms, and joined support groups to connect with others navigating adrenal insufficiency symptoms. Hodge’s trying journey to diagnosis isn’t uncommon, because the symptoms are difficult to spot.

“It is very challenging to diagnose adrenal insufficiency because the symptoms are so nonspecific,” says Paul Sack, MD, the Chief of the Division of Endocrinology and Metabolism at MedStar Hospital in Baltimore, “However, it is essential that we make the correct diagnosis and give the medications appropriately.” While only an endocrinologist can make that diagnosis, there are some signs of adrenal insufficiency you can look out for.
What is Addison’s Disease?
To understand Addison’s disease, we first have to dive into the role of two small, but mighty glands: the adrenal glands. “The adrenal glands are small hormone producing glands that sit directly above the kidneys on both sides,” says Dr. Sack. They produce multiple hormones (i.e. estrogen, testosterone, adrenaline, and noradrenaline), but the two we’re concerned with today are cortisol and aldosterone.
Cortisol helps regulate metabolism and turn food into usable energy, as discussed below, while aldosterone can balance salt and fluid levels in the body, and both help keep blood pressure normal, which are all pretty important tasks for staying healthy. They’re also both in short supply when someone has Addison’s disease.
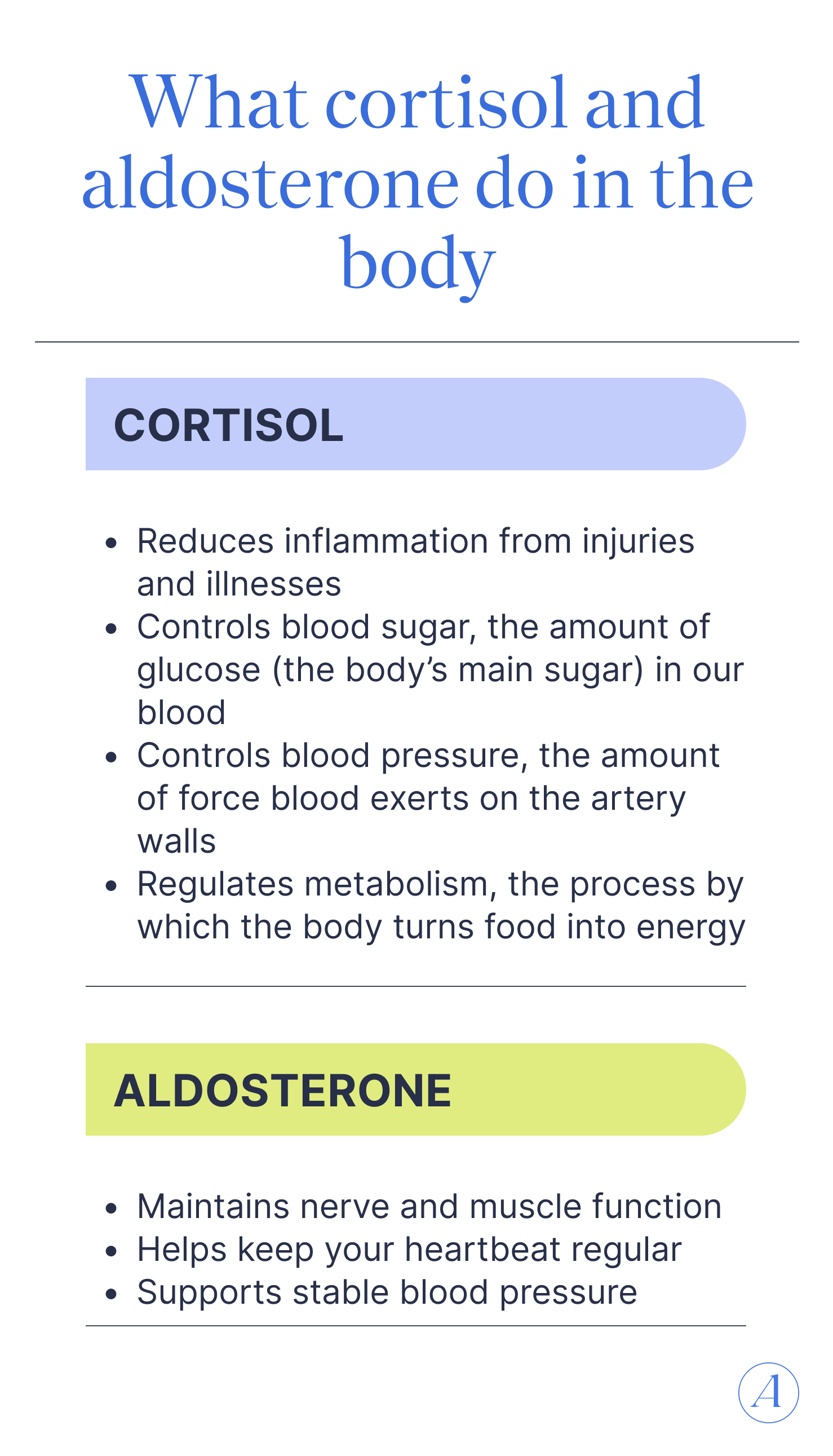
If you’ve seen the viral “lower your cortisol levels” videos on social media, less cortisol may sound like a good thing. After all, cortisol is often referred to as “stress hormone.” But cortisol’s bad rep isn’t warranted. It does help regulate our stress response but it also helps:
- Reduce inflammation from injuries and illnesses
- Control blood sugar, the amount of glucose (the body’s main sugar) in our blood
- Control blood pressure, the amount of force blood exerts on the artery walls
- Regulate metabolism, the process by which the body turns food into energy
Addison’s disease also impacts the less hyped, but equally important hormone aldosterone. This hormone’s main role is to regulate sodium (aka salt) and potassium levels, which together:
- Maintain nerve and muscle function
- Help keep your heartbeat regularly
- Support stable blood pressure
Types of adrenal insufficiencies
There are three main types of adrenal insufficiency: primary, secondary, and tertiary. Addison’s disease specifically denotes primary adrenal insufficiency. Each of the three types has a distinct reason why the adrenal glands aren’t producing enough cortisol and aldosterone:
- Primary adrenal insufficiency: When there’s direct damage to the adrenal glands, meaning they can’t produce enough of these hormones.
- Secondary adrenal insufficiency: When the pituitary gland, a small gland at the base of the brain, doesn’t make enough adrenocorticotropin (ACTH), which is the hormone that tells the adrenal gland how much cortisol and aldosterone to make.
- Tertiary adrenal insufficiency: If you’re ever played a game of telephone, you know how easy it is for a message to get lost along the way. Tertiary adrenal insufficiency is similar, since this type occurs when the hypothalamus doesn’t make enough corticotropin-releasing hormone (CRH), a hormone that tells the pituitary gland to make ACTH, which then tells the adrenal glands to produce cortisol.
In this article, we’re specifically focusing on Addison’s disease (primary adrenal insufficiency); while secondary and tertiary might have similar symptoms, the causes and treatments are different. A healthcare provider (usually an endocrinologist) will diagnose the type and adjust your treatment plan accordingly.
Early symptoms of Addison’s Disease
Now that we understand what Addison’s disease is, what exactly does it look and feel like? “Assuming that the cause is autoimmune, the earliest symptoms may be very subtle. This can just be fatigue, nausea, loose bowels,” says Dr. Sack, “One of the difficulties with making the diagnosis is that there is not one symptom to look for.” He adds that as cortisol and aldosterone levels dip, symptoms become more pronounced.
The most common symptoms, whether early on or later, include chronic fatigue, weakness and pain, weight loss, and digestive issues. Addison’s disease can also cause mood changes, menstrual irregularities, dizziness, salt cravings, as well as skin changes.
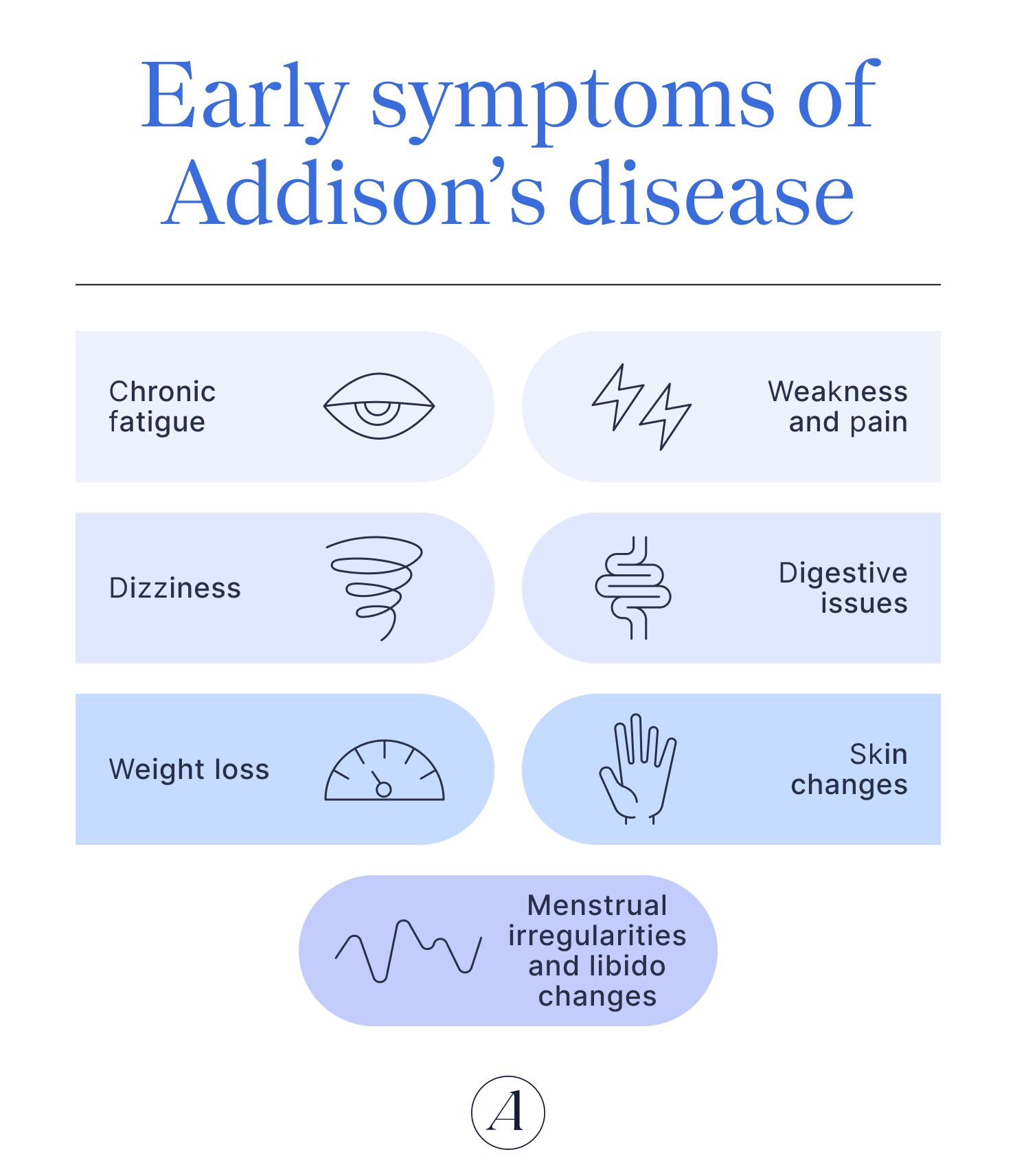
Chronic fatigue
Have you ever felt physically tired or like you were lacking energy? For most of us, the answer is probably yes, and this sensation is often what fatigue feels like. It’s important to know that varying levels of fatigue can be a normal reaction to an intense workout or a long day at work. Chronic fatigue comes into play when someone is experiencing severe fatigue that becomes a constant companion day in and day out; this may be a sign of something more serious.
There are many reasons chronic fatigue can occur, and Addison’s disease is quite rare (Addison’s patients typically experience very extreme fatigue levels). Hypothyroidism, hyperthyroidism, iron deficiency, diabetes, depression, and chronic fatigue syndrome can also lead to fatigue, and this isn’t an exhaustive list of potential causes.
The reason Addison’s causes chronic fatigue stems from cortisol's role in helping to produce enough energy. When our bodies can’t produce enough energy, we often feel fatigue that can’t be fixed by rest alone.
Weakness and pain
Another common symptom is weakness or pain in the muscles or joints. This symptom stems from the reduced production of aldosterone which, if you remember from above, balances electrolytes (i.e. sodium and potassium) in the body. Electrolytes aren’t just a buzzword for sports drinks; they are important for normal nerve and muscle functioning.
There’s many different forms muscle weakness or pain can take, depending on severity and the individual:
- Muscle pain
- Muscle spasms
- Joint pain
- Joint stiffness
Salt cravings
Remember how aldosterone regulates sodium and liquids? If Addison’s disease disrupts aldosterone production, someone can experience salt cravings since these levels aren’t regulated as intended.
Dizziness
Dehydration isn’t the only reason Addison’s disease might cause dizziness. Low blood sugar (hypoglycemia) related to inadequate amounts of cortisol and aldosterone can cause someone to feel lightheaded as well. In severe cases, this can lead to fainting or losing consciousness.
Digestive issues
Cortisol plays a role in metabolism and inflammation. If the adrenal glands don’t produce enough cortisol, it could have an impact on the digestive system, leading to symptoms like:
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Loss of appetite
- Stomach cramps
If these symptoms sound similar to gastrointestinal issues, like IBS, or viral stomach bugs, it’s because they are. These similarities are one of the reasons Addison’s disease may be misdiagnosed as something else.
Weight loss
When you lose weight unintentionally, characterized as dropping 5% or more of your bodyweight in less than a year without changing diet or lifestyle, it’s usually a sign of an untreated medical issue. Addison’s disease may be to blame, because cortisol levels help us maintain a healthy appetite.
But may is the keyword here since unintentional weight loss has many potential causes, ranging from stress to Celiac disease to certain types of cancer. A healthcare provider usually needs to assess symptoms and run tests to determine the exact cause.
Skin changes
If a doctor suspects Addison’s disease, they may search for any hyperpigmentation, an area or spot on the skin that’s noticeably darker.
The hyperpigmentation could be anywhere on the body but is most commonly found in the:
- Lines on the palms
- Gums
- Lips, particularly where the lips meet the skin
- Elbows
- Knuckles
- Posterior neck
- Breast nipples and the darker area surrounding them
- Nail beds
Hyperpigmentation may also be found all over the skin, something Dr. Sack refers to as a bronzing of the skin. He says it often looks like getting a good tan all over, not just in areas exposed to sunlight.
“When the cortisol levels start to decline, the normal response is for the pituitary gland to try to get the levels back up,” he explains. This prompts it to make more ACTH, which is secreted with another hormone, melanocyte stimulating hormone (MSH). Dr. Sack adds, “This hormone prompts melanocytes in the skin to darken the skin.”
Menstrual irregularities and libido changes
A lower libido might not seem like it’s related to Addison’s disease, but it can be. In fact, one study found 41% of women and 59% of men with adrenal insufficiency reported not being able to or not enjoying sexual activities. This may be due to chronic fatigue and lack of energy, though the right amount of cortisol (i.e. not too much or too little) does seem to aid the ability to have an erection or to support natural vaginal lubrication.
For those who menstruate, Addison’s disease may cause irregular periods, though there’s a lack of research on why (though hopefully that gap is filled soon!).
Signs of adrenal crisis: When symptoms become an emergency
If cortisol and aldosterone production drops too much, someone could enter an adrenal crisis or an Addisonian crisis. This is a life threatening emergency which often includes symptoms like stomach pain, dizziness, and vomiting. It may rapidly lead to shock, a coma, or metabolic encephalopathy, a brain disorder caused by metabolic issues.
“Adrenal crises feel very scary, and you genuinely feel like you are dying,” explains Hodge, “My first crisis was when I was diagnosed. I had developed the disease and didn't have enough cortisol in my body.”
Since then, Hodge has had two other crises, once when she couldn’t get a proper dose of her medication when traveling and third when she had the stomach flu. Thankfully, she could access emergency medical treatment during these three crises, which is an important step if you spot any warning signs of an adrenal crisis, such as extreme dizziness or vomiting.
How to test for Addison’s Disease
If you suspect you have Addison’s disease, an endocrinologist can make a diagnosis. Since Addison’s disease presents few symptoms in its early stages, your endocrinologist will most likely perform some tests alongside assessing your symptoms and medical history.
Dr. Sack details that he often orders lab work whenever someone presents with symptoms that could be due to Addison’s disease. “Specifically, we would do a morning cortisol level around 8 AM or earlier,” he explains, “This is when cortisol typically has its peak.”
Other common diagnostic tests include:
- ACTH stimulation test: a hormonal test where human-made ACTH (the hormone the pituitary gland produces to signal it’s time for cortisol production) is administered via an IV. Thirty minutes to an hour later, a medical professional will assess cortisol levels in the blood. If Addison’s disease isn’t present, cortisol levels will have risen. If it is present, there will be little to no increase in cortisol production.
- CT scans: A CT scan can reveal any abnormalities in the stomach, including enlarged or damaged adrenal glands. Many times, a CT scan will not be the gold standard for diagnosis, as it may appear normal.
- CRH stimulation test: This test is similar to the ACTH test in that human-made CRH is injected into the body. When Addison’s disease isn’t present, CRH will cue the pituitary gland to produce ACTH, which should then prompt the adrenal glands to produce cortisol and aldosterone. However, a CRH stimulation test is not recommended for routine evaluation of adrenal insufficiency.
How a specialist can help
When Addison’s disease is the diagnosed reason for symptoms, an endocrinologist can prescribe the right treatment, which usually includes hormone replacement medications. We often think of replacing estrogen and progesterone during menopause, but for Addison’s disease, it involves taking a daily dose of corticosteroids to replace the cortisol your body can’t produce.
However, it is essential to seek out an accurate diagnosis for your symptoms, because taking corticosteroids without the correct diagnosis can be detrimental to your health; these medications come with side effects and should only be prescribed for patients who truly need them. If you don’t have a trusted provider, services like Allara can provide you with a referral to an endocrinologist in your area and can also support you with ongoing virtual care.
After Hodge’s first adrenal crisis, her doctor prescribed hydrocortisone, a type of corticosteroid. Hydrocortisone has both cortisol and aldosterone effects, which is why it is the preferred treatment for Addison’s. “It is a lot like diabetes in that I have to take it several times a day to try to mimic how my body would release it if it could,” says Hodge, “I also carry an emergency injection at all times, wear a medical ID bracelet, and have instructions for what to do if I have a crisis in my wallet.”
Dr. Sack adds that education is often a crucial part of treatment, since the amount of steroids someone takes may need to be adjusted for certain situations, such as if they’re getting surgery, and because wearing a medical ID bracelet and having written instructions are essential if someone requires emergency medical help when unconscious. He adds, “We also make sure that patients have injectable steroids for home in case they cannot keep down their oral medications.”
Key takeaways
- Addison’s disease is a rare and difficult to diagnose conditions where the adrenal glands don’t produce enough cortisol and aldosterone.
- Common symptoms of Addison’s disease include chronic fatigue, muscle weakness or pain, salt cravings, dehydration, dizziness, digestive issues, unexplained weight loss, skin changes, and menstrual irregularities.
- Symptoms alone aren’t enough to diagnose Addison’s disease. A qualified endocrinologist, like the ones at Allara, can assess your medical history, refer you to an in-person provider for diagnostic testing, and help manage and provide a treatment plan virtually.
Frequently Asked Questions (FAQs)
What is adrenal insufficiency?
Adrenal insufficiency is when the adrenal glands, small glands that sit on top of the kidneys, don’t produce enough cortisol and aldosterone. While cortisol is best known as the “stress hormone,” it’s also important for overall health, helping to turn food into energy, regulate blood sugar levels and blood pressure, and more. Aldosterone also plays a role in blood sugar and blood pressure regulation as well. When the body doesn’t have enough of these hormones, someone can experience symptoms ranging from chronic fatigue and unexplained weight loss to shock or fainting.
What is it like to live with Addison's disease?
Living with Addison’s disease often means taking a corticosteroid medication for the rest of your life in order to keep cortisol levels in a healthy range. When the condition is managed, either through steroids or another treatment, people with Addison’s disease can live a relatively active life with a normal life expectancy.
What causes low cortisol levels?
Damage to the adrenal glands, autoimmune issues, or problems with the pituitary gland or hypothalamus, two parts of the brain that are involved in signaling to the adrenal gland that it needs to produce more cortisol, are some of the most common reasons for low cortisol levels. A doctor, usually an endocrinologist, can diagnose the exact cause.
How rare is Addison's disease?
Addison’s disease is rare, affecting about every one in 100,000 people. That said, it’s most likely underdiagnosed. Symptoms often don’t present until later stages of the disease, and they are often confused for a variety of other conditions, ranging from IBS to depression.












