
Hormone balance 101: Your guide to feeling better every day
Hormones have natural rhythms that follow daily, monthly, and even lifetime patterns. When these fluctuations become dysregulated, you might develop unexplained symptoms that affect your health. Sometimes this is referred to as a hormonal imbalance. However, the term doesn’t quite fit. Here’s why and how you can support your natural hormonal rhythms.
The word “balance” gets tossed around a lot regarding the topic of hormonal health for people assigned female at birth. So naturally you may be wondering what hormone balance looks like.
The concept is a bit misleading though. Our sex hormones naturally fluctuate throughout our lives, from puberty through our reproductive years, and into perimenopause, menopause, and beyond. And, for those with a menstrual cycle, hormones fluctuate throughout the month. Some hormonal changes even occur throughout the day, shifting from morning to night.
“For women, hormonal fluctuations are a natural and essential part of daily physiologic processes, with each hormone intricately linked and influencing one another,” says Gouri Pimputkar, DO, a board-certified OB/GYN at Allara. “By stating that ‘hormones are not balanced,’ this implies that there is something broken or gone wrong. When in reality, hormones fluctuate naturally due to stress, diet, sleep, age, and overall health.”
So why do articles and social media posts and self-help books bring up hormonal balance? Do our hormones exist on a proverbial teeter-totter, like the ones we used to play on at the park or school recess? Not exactly.
However, when one hormone increases or decreases beyond a normal or optimal range, it can indeed affect other hormone levels, leading to frustrating symptoms or contributing to endocrine disorders, such as polycystic ovary syndrome (PCOS).
Instead of thinking about hormones as needing balancing, you may find the concept of optimization or support to be more helpful. When we support our hormones with healthy lifestyle changes, supplements if needed, and any necessary medical interventions, we can better optimize them to work well in concert with each other.
Myth-busting hormone “balance”
Exploring a few concepts about hormones can help illuminate why the idea of hormone balance is a bit of a myth, but also where the concepts of support or optimization—rather than balance—can come into play.
“There are conditions where hormones are not functioning to the best of their capacity, and therefore resulting in a host of symptoms,” Dr. Pimputkar says. “Ultimately, what may seem ‘balanced’ for one individual might not be the same for another, thus emphasizing the need for a personalized approach to hormonal health.”
“Every single hormone is one of countless messengers within the body,” adds Felice Ramallo, MS RD, lead dietitian at Allara Health. “These messengers fluctuate as needed throughout the day, and per circadian (24-hour) and infradian (monthly) rhythms in female bodies. This means that hormonal 'balance' is a constantly moving target, with several influencing factors.”
This section discusses, daily, monthly, and lifetime hormonal fluctuations and provides examples of potential disruptions to usual hormonal patterns, along with examples of optimization.
Hormonal fluctuations throughout the day
Some of our hormones have what’s called a circadian rhythm, meaning they follow a 24-hour cycle. Examples include melatonin, cortisol, and estrogen, to name a few.
- Melatonin (aka the “sleep hormone”) increases in the late evening because of darkness cues and then declines with daylight cues.
- Cortisol (aka the “stress hormone”) generally peaks in the morning, giving you some get-up-and-go, and decreases throughout the day, with a few exceptions.
- Estrogen (often called a “female hormone,” though it’s necessary for the male body too) peaks in the morning and undergoes a natural drop as the day progresses.
Disruption example: Several factors can disrupt these patterns, including altered sleep schedules from shift work, jet lag, and more. And issues can arise when one of these hormones unexpectedly shifts. For example, cortisol suppresses melatonin. So if your cortisol level remains elevated, say from chronic stress, you might have difficulty falling asleep with less melatonin to help you.
Optimization example: That doesn’t mean you have to somehow perfectly balance cortisol and melatonin on a proverbial hormonal seesaw, but reducing your stress level may support not only issues with cortisol but also melatonin.
Hormonal fluctuations throughout a month
When considering the menstrual cycle, your hormone levels also change throughout the month. This is because your brain and your ovaries communicate in a feedback loop via the hypothalamic-pituitary-gonadal (HPG) axis.
“Each hormone informs another,” Ramallo says. “Our sex hormones, especially, are part of a coordinated signal cascade that constantly flows between follicular and luteal phases, each with hormone peaks and valleys of their own.”
Our menstrual cycles have two main phases, with ovulation offering a transition between the two. During these phases, hormone levels follow a distinct pattern. As an example, progesterone is low during the follicular phase, but it rises and falls in the luteal phase.
- Follicular phase: Begins at the start of menstruation and lasts into ovulation.
- Luteal phase: Begins during ovulation and lasts until menstruation.
“When helping patients achieve hormone balance,” Ramallo, says, “what we are really trying to do is help them flow between parts of their cycle with minimal symptoms or disruptions to their quality of life. This process embraces the ever-changing seasons in one’s cycle. The same things don’t work for everyone. However, most people need elements of adding and pulling back throughout their natural cycle, to truly feel in harmony with it.”
Disruption example: Many factors can disrupt the usual trajectory of your reproductive hormones during your menstrual cycle. For example, high androgen levels (such as testosterone) can suppress luteinizing hormone (LH), which can then suppress ovulation.
Optimization example: Rather than equally balancing levels of testosterone and LH, one approach for supporting the menstrual cycle would be to find ways (under the guidance of a healthcare provider) to reduce androgen production in the ovaries to a more optimal level, which may then restore ovulation.
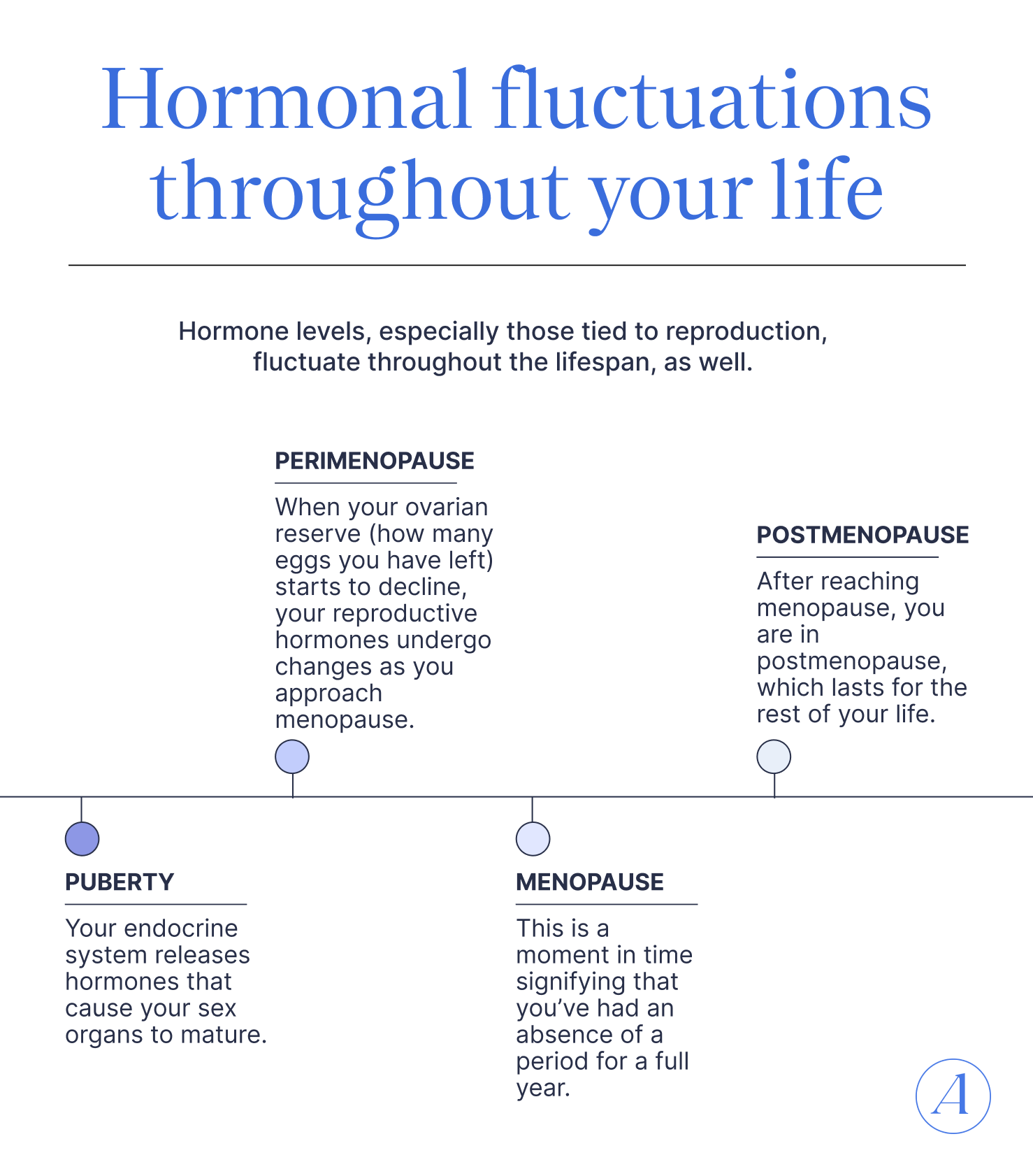
Hormonal fluctuations throughout your life
Hormone levels, especially those tied to reproduction, fluctuate throughout the lifespan, as well.
- Puberty: Your endocrine system releases hormones that cause your sex organs to mature.
- Perimenopause: When your ovarian reserve (how many eggs you have left) starts to decline, your reproductive hormones undergo changes as you approach menopause.
- Menopause: This is a moment in time signifying that you’ve had an absence of a period for a full year. From two years before your final menstrual period to two years after, your estrogen levels will have undergone a decline of more than 50%.
- Postmenopause: After reaching menopause, you are in postmenopause, which lasts for the rest of your life. Estrogen levels tend to stabilize once you’re two or more years beyond your final menstrual period.
Disruption example: Perimenopause may bring about symptoms, such as hot flashes, night sweats, mood changes, sexual dysfunction, vaginal dryness, and more because of fluctuating hormones or declining levels.
Optimization example: Optimization in cases of the menopause transition may involve supporting hormone levels with hormone therapy (MHT/HRT) for hot flashes, night sweats, and the prevention of osteoporosis. Certain lifestyle changes can also help ease symptoms.
Natural ways to support hormone health
Whether you’re experiencing hormone disruptions and their symptoms or feeling great, healthy lifestyle changes can support your hormonal health—and overall health—throughout all life stages.
Any discussion about lifestyle changes to balance hormones naturally needs to come with a side of practicality though. When you’re already dealing with frustrating symptoms, or you’re experiencing stress from daily life (who isn’t?) or you have a busy schedule, then lifestyle changes might feel harder to incorporate until you get into the swing of them.
One good rule of thumb is to start low and go slow, meaning you don’t have to make all these changes all at once or in an extreme way. In fact, going to extremes, such as intensive intentional weight-loss measures, can have the opposite effect and disrupt hormonal health.
Nutrition
Some nutritional changes can help support your hormones, but they don’t need to be extreme. Small changes are easier to sustain, and they add up to big health gains in the long run.
Take an intuitive or cyclical approach
“It all starts with listening to your body,” Ramallo says. “Our dietitian team is phenomenal at deciphering the clues and symptoms patients are coming in with to fill individual gaps. Much of this comes back to identifying places to add or pull back through the cycle.”
If you still have a menstrual cycle, your energy level and needs will fluctuate across the phases. For example, you might feel more energetic during your follicular phase, especially as you approach ovulation, thanks to a surge in estrogen. Feeling higher energy may translate to expending more energy, so you may need a nutrient boost. “You might need more complex carbs from starchy veggies, whole grains, and fruits to power you through and prevent blood sugar crashes,” Ramallo says.
Likewise, you may experience more fatigue, crashes, and cravings in the luteal phase or during menstruation. “This could be an opportunity to boost protein and fiber with beans, nuts, and seeds to regulate blood sugar and boost satiety,” she adds.
- Practical tip: Track how you feel across your cycle to help determine when your natural energy surges and slumps occur. Then adjust your diet accordingly. A registered dietitian can be a great help in identifying your patterns and needs.
Add antioxidant-rich foods
“We know that antioxidant foods are crucial to hormone health,” Ramallo says. “Getting plenty of leafy veggies, berries, seeds, beans, omega-3 rich fish, and functional foods like cacao or green tea/matcha is always a supportive measure.”
- Practical tip: Eat a rainbow of fruits and vegetables throughout each week.
Increase whole foods and decrease sugars
Ultra-processed foods often contain high amounts of added sugar, chemical preservatives, endocrine-disrupting chemicals that can impact hormonal function, and artificial flavorings designed to make you crave them.
- Practical tip: Follow the 80/20 rule. Get 80% or more of your food from whole food sources or foods with a short ingredient list, reserving a little wiggle room (20% or less) for when convenience, cravings, or a celebration (cake, anyone?) wins out and you grab an ultra-processed food.
Eat for more stable blood sugar
How your body manages glucose (aka blood sugar) and insulin (see the insulin section below) can have an impact on your hormones. Eating for stable blood sugar means minimizing large glucose spikes, often from refined carbohydrates, such as white rice, pasta, and breads (that aren’t whole grain). This can help keep you more insulin sensitive (a good thing).
The postmenopausal stage can increase insulin resistance, which puts you at risk for health issues, such as type 2 diabetes or cardiovascular disease.
- Practical tip: Pair any refined carbohydrates or high-glycemic foods with fiber, protein, or healthy fats. These nutrients help slow glucose absorption in the bloodstream, potentially blunting glucose spikes and counteracting insulin resistance.
Prioritize protein
Amino acids are the building blocks of protein. We need nine essential amino acids from our diet, since the body cannot make them. Adequate protein intake is crucial for supporting hormonal health, since your body needs them to make certain hormones.
Protein, in combination with resistance training, helps build and preserve muscle, something we naturally lose as we age, unless we take steps to counteract the decline in muscle mass. Protein needs vary, but the minimum amount the body needs to function is about 0.4 grams of protein per pound of body weight per day. But experts say that’s not enough for many people and that aiming for 0.6 to 1 gram of protein per pound is more ideal.
- Practical tip: Get 30 to 40 grams of protein per meal whenever possible.
Supplements
Your needs will differ from someone else’s, and you may not even need any at all.
“In general,” Dr. Pimputkar says, “the rule of thumb is to trust science, evidence-based information and providers who are comfortable managing both medical and supplement treatments.”
“For years, I have recommended a number of supplements to get down to the unique nutrient needs of every patient,” Ramallo adds. “Several of my recommendations now come together in the Allara Hormone Equilibrium supplement. We’ve created it for this very reason.”
Here are a few ingredients or supplements to ask your healthcare provider about.
Inositol
“One of the most foundational nutrients for anyone needing more hormonal support, is inositol,” Ramallo says. “It acts as a secondary messenger for sex hormones, thyroid hormone, and insulin. It meets the wide range of concerns that we often face in women's health. There are heaps of evidence for its use at several life stages from our time in the womb, through menopause.”
Vitamin D
“Vitamin D is one of the most integral vitamins in hormonal regulation, because of the ways that it manages the production of several of our hormones,” Ramallo says. “Name a body function, and there’s a role for D. It helps with estrogen and progesterone regulation. It increases the insulin sensitivity of our cells. It has a crucial influence on the hormones affecting bone health. The list goes on.”
Omega 3 fatty acids
Dr. Pimputkar recommends these anti-inflammatory powerhouses, which help improve insulin sensitivity, regulate androgen production, and more.
Exercise
Movement in general can be beneficial to overall health and support hormonal health. Although an intense bout of exercise can temporarily spike cortisol, regular exercise, in moderation, can help increase your resilience to stress, which helps to regulate levels of the stress hormone. To be clear, all levels of exercise (intense, moderate, and gentle) can be beneficial, but overdoing intensity can backfire.
Strength training can be particularly beneficial for regulating blood sugar levels and making you more insulin sensitive. This is because muscle, when contracting, acts like a sponge for excess glucose, without the need for insulin. Hyperinsulinemia, a high insulin level, is associated with PCOS.
Also keep in mind that the phases of your menstrual cycle can impact your energy levels and performance. For example, you may feel more get-up-and-go or that you can lift heavier during the follicular phase, especially as you get closer to ovulation. “This is a great opportunity to capitalize on higher tolerance for physical activity, strain, and stress,” Ramallo says.
Likewise, you may feel more fatigued during the luteal phase. “One can be more sensitive to stress or exertion during these periods of time,” she adds, “so an emphasis on gentle movement can be a better way to keep your body moving while allowing for rest and recovery.”
- Practical tip: Find activities you love, whether hiking, swimming, running, cycling, etc. And aim for at least two resistance-training workouts per week. If you’ve got a busy week, focus on those muscle-building workouts over others.
Sleep
“Sleep is not only a time where our body rests and restores,” Dr. Pimputkar says, “but it is a time when we function at a decreased metabolic demand allowing for a reset of important hormonal activities.”
Aim for getting seven hours of quality sleep per night whenever possible, with the caveat that doing so can be easier said than done. If you’re having trouble sleeping, don’t hesitate to talk to your healthcare provider.
During your luteal phase, when energy levels can tank, you may need to prioritize sleep even more. “Sometimes, sleep habits need a reevaluation during this time,” Ramallo says, “and we might recommend a more consistent sleep and wake time or more time spent in bed.”
- Practical tip: Block out light and noise pollution with an eye mask or blackout curtains for the former and a white- or pink-noise machine for the latter.
Stress management
Your body’s reaction to stress, that fight-or-flight response, exists to keep you safe when you encounter a threat, such as an off-leash dog coming after you on your walk. However, sometimes we experience ongoing stress from having an extensive to-do list, a litany of work demands, distressing relationship issues, etc.
Cortisol naturally shifts throughout the day, but it can become dysregulated when chronic stress ensues, impacting many facets of health including sleep, which is crucial for hormonal health. That’s why finding ways to reduce stress is crucial. Underlying health conditions can also cause irregularities in cortisol, so never hesitate to talk to a provider.
- Practical tip: When stress crops up, try a box breathing exercise to get you out of that fight-or-flight state. Picture a square, and designate one side of it for each of the following: inhale for a count of five, hold for a count of five, exhale for a count of five, and hold for a count of five before repeating.
How hormonal issues show up in the body
As you read through this list of potential hormonal issues, you may notice that symptoms of one hormonal disturbance overlap with others and that symptoms in general are nonspecific, meaning they could apply to other underlying conditions. That’s why if you are experiencing any unexplained symptoms that are distressing or affecting your quality of life, you should talk to a doctor.
Estrogen
What it does: Estrogen is an umbrella term for a family of similar hormones, with estradiol (E2) the most abundant during your reproductive years.
- Regulates the menstrual cycle
- Develops and supports reproductive organs
- Promotes breast growth and milk production
- Increases bone density and reduces risk for osteoporosis
- Protects against cardiovascular disease
- Supports mood and cognitive function
- Regulates body temperature
- Helps maintain insulin sensitivity
Potential signs of high levels:
- Irregular menstrual cycle
- Pelvic pain
- Breast changes
- Unexplained weight gain
- Mood changes
- Headaches
- Fatigue
- Digestive issues
- Sleep problems
Potential signs of low levels:
- Hot flashes
- Night sweats
- Vaginal dryness
- Sexual dysfunction
- Mood changes
- Cognitive issues
- Irregular or absent periods
- Sleep disturbances
- Dry or thinning skin
- Unexplained weight gain
Progesterone
What it does: Progesterone is a key hormone for the menstrual cycle and pregnancy.
- Regulates parts of the menstrual cycle
- Thickens the lining of the uterus in preparation for a potential pregnancy (after ovulation)
- Maintains the uterine lining during pregnancy
- Supports placental development
- Promotes breast development and milk production
- Balances the effects of estrogen
- Regulates body temperature
- Regulates mood
- Plays a role in cognitive health
- Reduces inflammation
- Supports bone health
Potential signs of high levels:
- Mastalgia (breast pain or tenderness)
- Fatigue
- Gastrointestinal changes (e.g., bloating, nausea, constipation)
- Weight changes
- Mood changes
- Sexual dysfunction
- Irregular periods
- Acne
Potential signs of low levels:
- Menstrual irregularities
- Infertility
- Recurrent pregnancy loss
- Mood changes
- Fatigue
- Headaches or migraine attacks
- Sleep disturbances
- Unexplained weight gain
Cortisol
What it does: Cortisol is a stress hormone that fluctuates throughout the day. It’s necessary for your immune system, sleep-wake cycle, and more. It can become dysregulated during times of chronic stress. But some conditions can also chronically elevate cortisol and require medical intervention.
- Increases blood pressure
- Elevates blood sugar
- Increases insulin resistance
- Regulates metabolism
- Suppresses the immune system during stress
Potential signs of abnormal high levels:
- Unexplained weight gain
- High blood pressure
- High blood sugar
- Increased cravings
- Easy bruising
- Slow wound healing
- Muscle weakness
- Increased hair growth on the face or body
- Mood changes
- Increased thirst or urination
- Irregular menstrual cycles
- Pelvic pain
Potential signs of abnormal low levels:
- Chronic fatigue
- Muscle weakness
- Loss of appetite
- Vomiting
- Diarrhea
- Unexplained weight loss
- Abdominal pain
- Skin darkening
- Dizziness upon standing
- Salt cravings
- Confusion
- Low blood pressure
Thyroid hormone
What it does: Thyroid hormone is a group of hormones your thyroid gland produces, including Thyroxine (T4) and Triiodothyronine (T3). Hyperthyroidism (an overactive thyroid gland) will produce high thyroid hormone levels. And hypothyroidism (an underactive thyroid gland) will produce low thyroid hormone levels.
Potential signs of high levels:
- Rapid heart rate
- High blood pressure
- Shakiness
- Feeling anxious
- Weight loss
- Decreased appetite
- Diarrhea
- Sleep disturbances
- Menstrual cycle changes
- Swelling of the neck or eyes
Potential signs of low levels:
- Fatigue
- Increased sensitivity to cold
- Constipation
- Dry skin
- Unexplained weight gain
- Puffy face
- Hoarse voice
- Coarse hair and skin
- Thinning hair
- Muscle weakness
- Slow heart rate
- Depression
- Cognitive issues
Testosterone
What it does: Although often considered a “male hormone,” testosterone also plays important roles in the female body. Testosterone levels can refer to free or total testosterone. Most testosterone in the body is bound to proteins. Free testosterone is the type that your body can readily use. Testosterone is an androgen, and high levels of androgen can signal PCOS.
- Regulates libido
- Boosts mood
- Boosts cognitive function
- Supports bone health
- Helps build and maintain muscle
- Supports metabolism
- Supports ovarian function
Potential signs of high levels:
- Irregular or absent periods
- Fertility issues
- Hirsutism (excess male-pattern hair growth)
- Hair loss
- Voice deepening
- Acne
- Increased muscle bulk (rare)
- clitoral enlargement (rare)
Potential signs of low levels:
- Low libido
- Fatigue
- Low mood
- Cognitive issues
- Decreased muscle strength
- Bone loss
Insulin
What it does: Insulin is a hormone your pancreas produces and secretes. It helps signal your cells to uptake glucose to be used for energy. Insulin resistance, when cells stop responding well to insulin’s signaling, is a common feature of PCOS. Insulin resistance can also develop or worsen when estrogen levels decrease.
Potential signs of high levels:
- High blood sugar
- High blood pressure
- Abnormal lipid levels (triglycerides or cholesterol)
- Fertility issues
- Irregular menstrual cycles
- Acne
- Hirsutism
- Weight gain
Potential signs of low levels:
- Shakiness
- Sweating
- Confusion
- Irregular heart beat
When to seek medical support
“In general, we know our bodies best,” says Dr. Pimputkar. “There are some tell-tale signs that could indicate a hormonal work up is needed.”
These include an irregular menstrual cycle or unexplained symptoms that warrant further evaluation. Pimputkar notes a few: “Fatigue, an increase in hair growth or acne in unwanted places, unexplained hair loss, weight fluctuations, sleep disturbances, mood changes around your period—the list can go on and on.”
The bottom line is that if you are experiencing frustrating health symptoms, don’t hesitate to reach out to a healthcare provider. “Find a provider who listens to you, understands your goals, and ultimately is here to help you live your healthiest, best life!” Dr. Pimputkar adds.
Key takeaways
- Our hormone levels naturally fluctuate daily, monthly (for females), and throughout our lifetimes.
- Since each hormone level affects other hormone levels, sometimes an abnormal level with one hormone can impact others. That doesn’t mean you necessarily have an imbalance.
- “Balancing” hormones is not about equalizing levels; rather it’s more about supporting your hormones with lifestyle changes and supplements and medications if necessary.
- If you’re experiencing unexplained symptoms, Allara can help.
FAQ
How do I balance my hormones?
Hormone levels naturally fluctuate throughout the day, and for people with a menstrual cycle they can fluctuate throughout the month, and for everyone, they change over the course of a lifetime. Each hormone acts as a chemical messenger, and one hormone can affect another hormone. So the concept of hormonal balance is complicated. In general, you can support your hormonal health by eating a balanced diet, regulating stress, prioritizing sleep, and engaging in physical activity. If you are experiencing symptoms suggestive of a hormonal issue, working with a knowledgeable healthcare provider can help.
What causes hormonal imbalance?
Hormone levels affect each other. So an abnormality with one hormone can cause an abnormality with another. However, our hormones can also fluctuate throughout the day and your lifetime, and for people with a menstrual cycle, hormones can also fluctuate monthly. These changes don’t necessarily reflect a hormonal imbalance. However, if you are experiencing unexplained symptoms, talking to a healthcare provider is always a good idea.
What are the signs of hormonal imbalance?
A hormonal imbalance may be present if you are experiencing menstrual cycle irregularities, fertility issues, unexplained symptoms that are affecting your quality of life, and more. If this is the case for you, reach out to a knowledgeable healthcare provider who can investigate and provide solutions.











