
How to test for PCOS (and what to expect)
Getting a PCOS diagnosis takes time and often involves several tests. No single test can confirm PCOS. Instead, healthcare providers use the Rotterdam criteria to evaluate menstrual cycles, androgens, and ovarian health. A comprehensive exam, blood work, and imaging will give the clearest picture of your hormonal and metabolic health.
Getting a PCOS diagnosis isn’t always a straightforward process, but that doesn’t mean it has to be a challenge either. Polycystic ovarian syndrome, or PCOS, is an endocrine condition that causes a wide variety of metabolic and hormonal symptoms. Often, people seek out care because they have symptoms that lead them to think they might have PCOS, like acne, increased facial and body hair, thinning scalp hair, midsection weight gain, and long menstrual cycles. Other times, people don’t realize they have PCOS until their healthcare provider suggests it as an explanation for less obvious symptoms like not getting pregnant within a year of trying.
No one test can definitively diagnose PCOS. Instead, your healthcare provider will utilize a variety of methods to get a full picture of your symptoms and then compare that to the diagnostic criteria for PCOS. Here’s what you can expect when getting a PCOS diagnosis.
What are the criteria for a PCOS diagnosis?
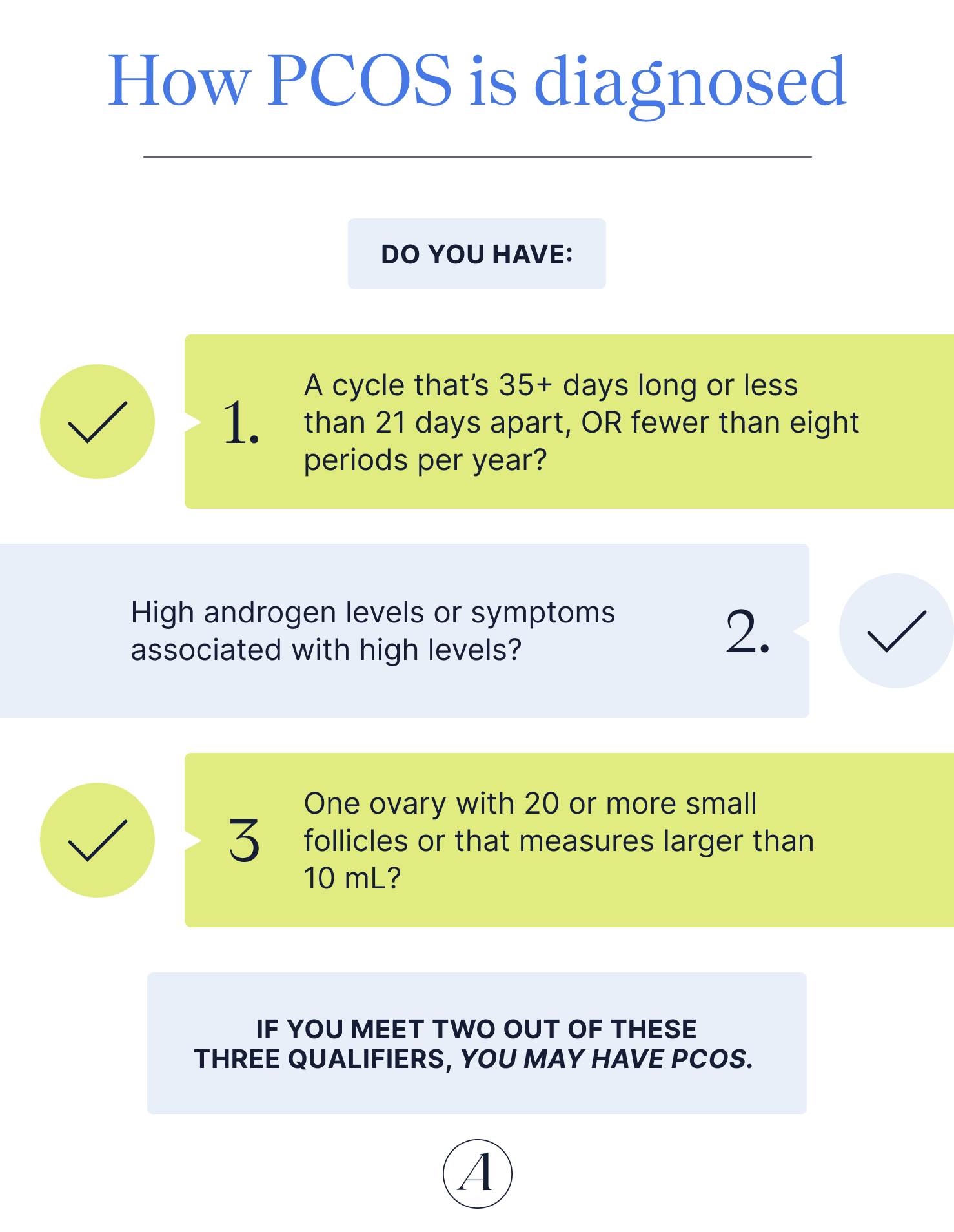
Healthcare providers use specific diagnostic criteria, known as the Rotterdam criteria, when diagnosing PCOS. To get a PCOS diagnosis, you must meet at least two of three criteria:
- Irregular menstrual cycles that are more than 35 days long or less than 21 days apart, OR those that have fewer than eight periods per year.
- High androgen levels (male sex hormones) or symptoms associated with high levels, such as acne, increased facial or body hair, and thinning scalp hair.
- Ovaries that look “polycystic” when viewed on ultrasound or a high antimullerian hormone level (AMH). To appear polycystic, at least one ovary should have 20 or more follicles measuring 2‐9 mm in diameter and/or an ovarian volume greater than 10 mL.
As part of your assessment, your healthcare provider will ask about any PCOS symptoms you may be experiencing as well as order a blood test to assess your hormone levels and an ultrasound to visualize your ovaries.
Getting a PCOS diagnosis requires:
- An evaluation of your symptoms
- Cycles 35+ days long or less than 21 days apart, OR fewer than eight periods per year
- A blood test
- High androgen levels or symptoms associated with high levels
- Ovarian imaging
- One ovary has 20 or more small follicles or measures larger than 10 mL.
- If you meet two out of the three, you may have PCOS.
What tests are used to diagnose PCOS?
The first stop on your PCOS journey is to see your healthcare provider. The first time you mention PCOS might be to your primary care provider or to your gynecologist.
“More often than not, a gynecology provider will make the diagnosis of PCOS,” says Gouri Pimputkar, DO, clinical lead at Allara Health. “A gynecologist typically will be able to address irregular periods and irregular ovulation, as well as help with treatment solutions for the symptoms of excess testosterone and insulin resistance.”
But gynecologists are not the only people on your care team who can diagnose PCOS. Endocrinologists, metabolic hormone specialists, and reproductive endocrinologists, physicians focused on reproductive hormones and conception, can also test for and diagnose PCOS.
“Which one to choose truly depends on your ultimate health goals, [your] connection with [the] provider, and what PCOS symptoms are most prominent,” says Pimputkar. “[Endocrinologists] are very helpful in managing the metabolic component of PCOS. Reproductive endocrinologists are the best of both worlds, where they can focus on ovulation to improve pregnancy, as well as the metabolic component.”
Your healthcare provider, regardless of their specialty, will utilize a variety of tests to assess whether you meet the diagnostic criteria and make their diagnosis.
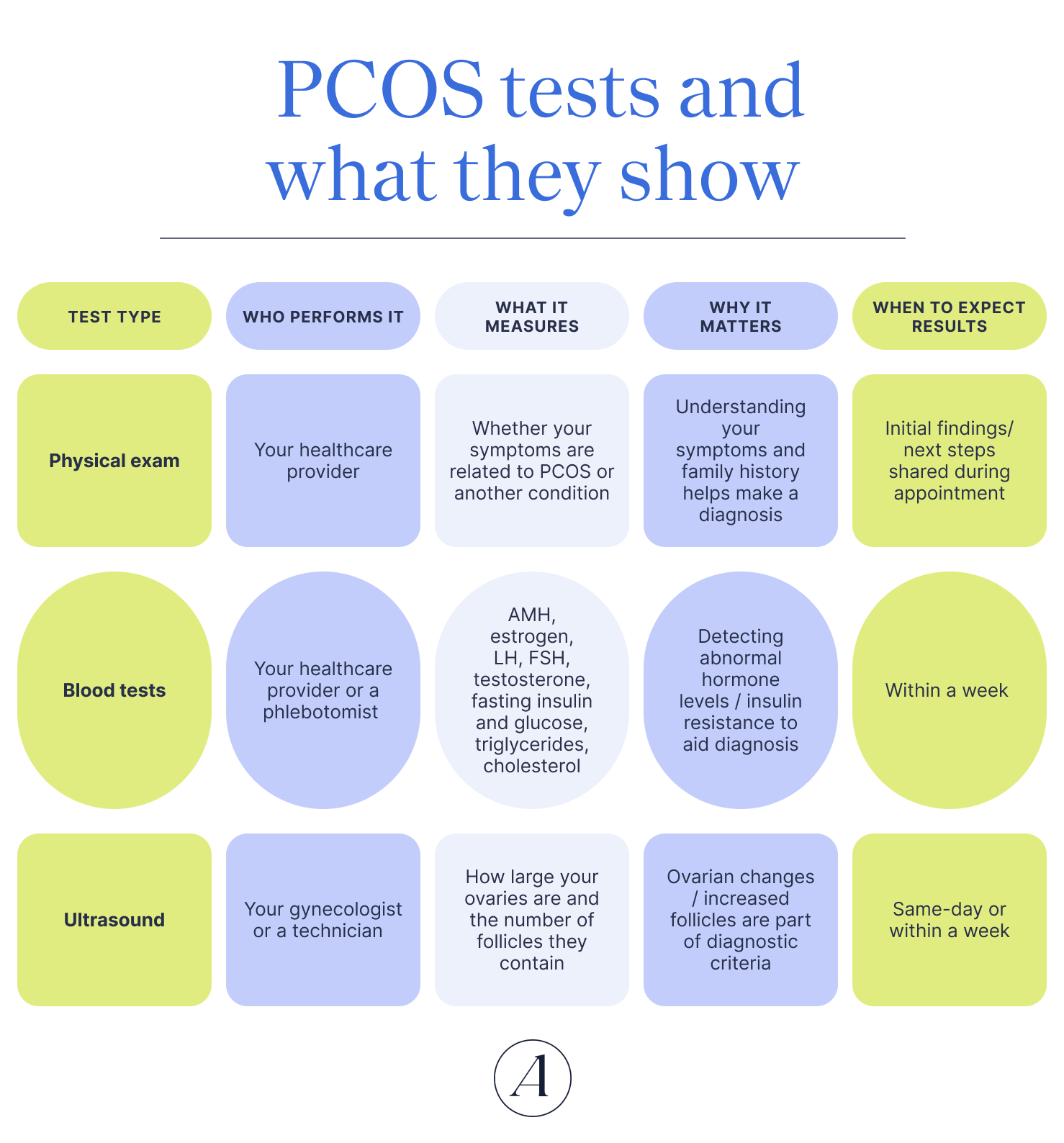
Physical exam
A physical exam and detailed medical history will help your healthcare provider determine whether your symptoms are related to PCOS or another condition.
Understanding your symptoms and any family history of PCOS can help your provider make a diagnosis.
Your provider will likely share their initial findings and any next steps during the appointment.
Blood tests
Your healthcare provider may draw labs or send you to a testing facility where a phlebotomist will draw your blood.
There are a variety of tests that can be helpful. These include measuring AMH, estrogen, LH, FSH, testosterone, fasting insulin and glucose, triglycerides, and cholesterol.
Abnormal hormone levels are part of the diagnostic criteria. Insulin resistance and metabolic issues are also common with PCOS.
Results typically come back within a week of getting your blood drawn.
Ultrasound
Your gynecologist may perform the ultrasound or send you to an imaging center, where a technician will perform the exam.
The test will look at your ovaries to measure how large they are and count the number of antral follicles they contain.
Changes to the ovaries, a larger volume or increased antral follicles, are part of the diagnostic criteria.
Depending on who performs the test, you may get results on the same day or within a week.
Medical exams
Your initial appointment will likely focus on your medical history and any symptoms you’ve been experiencing. Your healthcare provider will likely focus on questions that can help them assess whether you meet the diagnostic criteria. For example, they might ask when your last period was and if your periods are regular (every 35 days or fewer). If your cycles are longer than 35 days, or less than 21 days apart, OR you have eight or fewer periods per year, then you’d meet one of the criteria. Note that these criteria are for patients who are three or more years post-starting their first period; criteria for younger patients who are newly menstruating are different.
It’s important to note that if you use hormonal birth control, you may not know whether your cycle is regular. And that’s totally fine! Be sure to let your healthcare provider know what methods you’re using to control your cycle and how long you’ve been using them.
If you don’t track your periods, that’s OK too! Many people don’t take a closer look at their cycles until they are trying to conceive or they come off of hormonal birth control. Your healthcare provider will be able to assess your ovarian health regardless of whether you can remember how long your cycles are.
Some other questions your healthcare provider might ask include:
- Do you have any of the following symptoms: acne, weight gain, excess facial and/or body hair growth (hirsutism), or hair loss or thinning head hair
- When did your symptoms begin?
- Have your symptoms gotten worse or stayed consistent over time?
- Does anything improve or worsen your symptoms?
- Are you trying to become pregnant? If so, how long have you been trying to conceive?
Because there are multiple symptoms of PCOS, it’s a good idea to keep a journal (or even take notes on your phone) to keep track of changes. This way, you can follow, and remember, your symptoms over a defined period of time. You can then share this information with your healthcare professional in order to gain a deeper understanding of what is going on in your body.
Your healthcare provider may also conduct a visual exam to examine any physical symptoms of PCOS you might be experiencing. Some symptoms they might check for include cystic acne, facial and body hair growth, scalp hair loss, and darkened patches of skin around the groin and underarms — a sign of insulin resistance. If you’re seeing a gynecologist, they may also do an internal pelvic exam to rule out other issues that can cause similar symptoms.
And since there is a genetic component to PCOS, you’ll also want to know your family’s history. And not just your mom’s side! You can also inherit PCOS from your father’s side of the family. So even though your male relatives won’t have PCOS per se, if they carry the genes, they may have PCOS-like symptoms such as hormonal issues, receding hair, and insulin resistance.
Hormone blood tests
Blood tests can help identify any hormonal imbalances you might have. Your healthcare provider might draw your blood in their office or give you a prescription to do tests at an outside lab.
Depending on which hormones they want to test, you may need to go on a certain day of your cycle, repeat labs several times at different points in your cycle, or go early in the morning before you’ve had anything to eat.
Many blood test results usually come back within a week, often less, although testosterone tests can take a full two weeks. Some healthcare offices, like fertility clinics, can test hormone levels and have results back within the same day.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
FSH and LH are hormones produced by your pituitary gland that stimulate the ovaries to produce follicles. In a typical menstrual cycle, one of these follicles will continue developing and then ovulate and release an egg.
Typically, the ratio of LH to FSH is 1:2. But if you have PCOS, your LH levels can be twice or three times as high as your FSH. High LH levels can lead to high androgen levels, irregular egg development, and infrequent ovulation.
If you know where you are in your cycle, your healthcare provider may ask that you test your LH and FSH shortly after you get your period. LH rises around the time of ovulation, which means your LH might appear higher than it typically is if you test mid-cycle and happen to be ovulating.
Testosterone
A lot of people think of testosterone as a male hormone, but both sexes produce testosterone (and estrogen). Producing too much testosterone, a type of androgen, when you have ovaries, can lead to PCOS symptoms such as excess body hair, acne, and hair loss.
Having high androgen levels, or symptoms associated with high levels, is part of the diagnostic criteria for PCOS. So if your testosterone levels come back high, you’d meet another criterion.
Estrogen
People with PCOS often have high estrogen levels and insufficient progesterone, which can affect ovulation and make conception difficult. High estrogen levels alone aren’t part of the PCOS diagnostic criteria, but getting your estrogen checked is critical for understanding any hormonal imbalances you may have.
Because estrogen levels can fluctuate throughout your cycle, your healthcare provider may ask to check your estrogen on day three of your period (this is considered day three of your cycle) or multiple times throughout your cycle.
Antimullerian hormone (AMH)
Another hormone your healthcare provider may check is your AMH. AMH can be a helpful test if you are on hormonal contraceptives, since taking hormone-based medications can mask the hormone imbalance-related symptoms associated with PCOS. AMH is a test used to measure ovarian health and egg reserve. Your AMH decreases with age, and a higher AMH typically indicates a higher egg reserve.
People with PCOS tend to have a higher AMH than people without the condition. Studies suggest that an AMH level higher than 3.8–5 ng/mL can be indicative of PCOS.
Ultrasounds
A comprehensive evaluation for PCOS typically includes an ultrasound. Depending on the type of provider you see, they may perform the ultrasound in-office during your initial appointment, or they may refer you to a radiology facility. If your provider performs the ultrasound themselves, you may receive your results during the scan. If you have your imaging done elsewhere or have an ultrasound technician scan you, then you will likely have to wait a few days for your results to get sent to your healthcare provider.
To get a better visual of your ovaries, your provider or the technician will likely perform the ultrasound transvaginally. Transvaginal ultrasounds use a longer probe that gets inserted vaginally rather than used abdominally.
Transvaginal ultrasounds can be uncomfortable, especially if you experience pain with penetration. If you experience pain during your exam, let the person doing the scan know. You may be able to switch to an abdominal ultrasound, though it may not provide as clear an image of your ovaries.
If you know where you are in your cycle, or have somewhat predictable cycles, your provider may try to time your scan to the start of your cycle, when multiple small follicles, called antral follicles, are easiest to measure. If you have PCOS, you may have a higher-than-average antral follicle count.
The technician performing the scan will be looking for “polycystic morphology,” but the polycystic part of PCOS is a bit of a misnomer. The “cysts” are actually these antral follicles, small fluid-filled sacs that contain an egg each.
All typically functioning ovaries create multiple antral follicles per cycle. Then one follicle grows large enough to release an egg during ovulation. With PCOS, these follicles stop developing and remain small within the ovary. The average ovary contains 10-15 antral follicles at the start of each cycle. If you have PCOS, your ovaries may have more than 20 antral follicles each. This pattern of antral follicles is sometimes referred to as a “string of pearls” because of the way it appears on imaging.
You can still have an ultrasound if you use hormonal birth control, but your scans may not show a polycystic pattern. Getting a blood test to check your AMH can serve as an alternative here, as the Rotterdam criteria allow for either an increased antral follicle count, larger ovarian volume, or a high AMH. Note that birth control can potentially suppress AMH levels.
Though the ultrasound will focus on your ovaries, a comprehensive scan will also examine your uterus and cervix to rule out other conditions that can cause similar symptoms.
Cholesterol and glucose tests
If you get diagnosed with PCOS, your healthcare provider may order additional tests to assess your metabolic health. Remember, PCOS doesn’t just affect your reproductive health. PCOS is also associated with insulin resistance, high cholesterol, and metabolic syndrome.
“So much of PCOS is intertwined with metabolic dysfunction,” says Pimputkar. “It is important to evaluate fasting levels of insulin, glucose, and hemoglobin A1C. These labs check for insulin resistance, pre-diabetes, or even diabetes, which are very common for patients with PCOS.”
Some tests your provider might order include:
- Lipid profile: Lipid profiles check your cholesterol and triglycerides. People with PCOS tend to have higher cholesterol and triglyceride levels.
- Cholesterol is a type of fat. Ideally, your low-density lipoprotein (LDL) or “bad” cholesterol is low and your high-density lipoprotein (HDL), “good” cholesterol, is normal. People with PCOS tend to have higher LDL levels, which can lead to clogged arteries, blood clots, and heart attacks without intervention over time
- Triglycerides are another type of normally occurring fat. High triglyceride levels can increase the risk of type 2 diabetes, a condition that people with PCOS are more at risk of developing.
- Glucose test: This test measures the amount of glucose, or sugar, in your blood. Glucose tests are typically done first thing in the morning, fasting, before you have anything to eat or drink. High glucose levels can indicate insulin resistance, prediabetes, or diabetes.
- Fasting insulin: Given the link between insulin resistance and PCOS, your healthcare provider may order additional tests to assess insulin resistance even if your glucose levels are normal. A high fasting insulin level despite normal glucose tolerance can indicate insulin resistance.
- Hemoglobin A1c: This blood test shows your average blood sugar levels for the past two to three months. A high A1c can indicate prediabetes or diabetes.
After PCOS testing: What comes next?
What happens next depends on whether you get a PCOS diagnosis. If you don’t get a diagnosis or don’t meet enough of the criteria, that doesn’t necessarily mean you don’t have PCOS.
“It is always worth getting a second opinion if you are not sure about your diagnosis (or lack thereof),” says Pimputkar. “The diagnosis of PCOS can be made later in life if the symptoms, history, and lab and ultrasound results align with the criteria. With age and perimenopause/menopause, some features of PCOS may change or decrease.”
If you do get a PCOS diagnosis, the next step is developing a treatment plan. That treatment plan will depend on your symptoms and goals. For example, your treatment plan might look a lot different if you’re trying to conceive. Depending on your goals, your treatment plan will likely include a combination of lifestyle changes and medications. Lifestyle changes may include switching to a high-fiber diet and increasing physical activity. Medications may include metformin or over-the-counter supplements like inositol.
If testing reveals you have insulin resistance, your next steps might include following up with an endocrinologist, if you haven’t seen one yet. If you’re trying to conceive, your gynecologist might recommend meeting with a reproductive endocrinologist. Your care team might also include a registered dietitian, who can work with you to help simplify any dietary changes you might want to make.
Frequently Asked Questions (FAQs)
How do gynecologists check for PCOS
There are several ways a gynecologist can check for PCOS. First, they will likely take your medical history and ask about your symptoms. Next, they may do a pelvic exam and order an ultrasound. They will likely also order blood tests to check your hormone levels.
Does PCOS show up in blood work?
PCOS can show up on your blood work. Signs of PCOS might include high androgen levels, LH levels that are higher than your FSH, high AMH, high estrogen, and signs of insulin resistance, such as high blood glucose or high insulin levels. These values, by themselves, however, are not enough to diagnose PCOS.
Do you need to fast for a PCOS blood test?
Whether you need fast for PCOS-related blood tests depends on the tests. Hormone-based tests like AMH, estrogen, testosterone, LH, and FSH do not require fasting. Tests to check for insulin resistance, on the other hand, do require fasting.
Conclusion
PCOS is a complicated chronic condition with symptoms that can change over time. No two cases of PCOS are the same. Your biology is unique, and the way that PCOS manifests for you may be different than how it shows up in a friend, a family member, or anyone online. Getting a diagnosis can be a challenging, time-consuming endeavor, but knowing what’s going on with your body is worth it.
If you’re not sure about your doctor’s diagnosis, consider getting a second opinion. This is something we can help with at Allara. When it comes to your health, there’s no such thing as being too big an advocate for yourself.
Key Takeaways
- There’s no single test for PCOS. Healthcare providers evaluate your symptoms and use blood tests and ultrasounds to make a diagnosis.
- To get a PCOS diagnosis, you must meet at least two of three criteria: irregular menstrual cycles, symptoms of high androgens or high androgen levels, or polycystic-appearing ovaries.
- Gynecologists, endocrinologists, and reproductive endocrinologists can all diagnose and treat PCOS depending on your symptoms and health goals.
- Testing often includes hormone and metabolic screenings. These tests look for hormonal imbalances and signs of insulin resistance and other metabolic issues.











