
Managing PCOS pain: hormonal, pelvic, and digestive discomfort, explained
PCOS isn’t usually thought of as a painful condition, but for many people, it can cause discomfort ranging from pelvic pain to digestive issues and body aches. Because PCOS often overlaps with conditions, understanding the source of your pain is the key to feeling better.
Pain often isn’t thought of as one of the main symptoms of polycystic ovarian syndrome (PCOS) — but that doesn’t mean PCOS can’t cause pain. Many people living with PCOS report experiencing cramps, pelvic pain, digestive discomfort, and more.
There are different ways PCOS can cause pain and discomfort, and what that looks like can vary from person to person. PCOS can also co-occur with other conditions that can also cause pain like irritable bowel syndrome (IBS) and endometriosis. Unfortunately, PCOS pain is an underexplored area of research. But learning more about the different ways PCOS can present can help you identify whether your symptoms are typical or warrant further investigation.
What causes PCOS pain?
Understanding how PCOS affects the ovaries can help explain why PCOS can cause pain.
PCOS causes ovaries that look “polycystic.” While cysts are part of the name polycystic ovarian syndrome, the “cysts” caused by PCOS aren’t actually cysts; they’re follicles. Follicles are naturally-occurring fluid-filled sacs within the ovary that contain an egg each. Multiple follicles begin developing during the menstrual cycle, with one follicle ultimately growing large enough to release an egg during ovulation.
People with PCOS tend to have more of these follicles, often upwards of 20 follicles per ovary. However, these follicles often stop developing and remain small, less than 5-8mm. Having many of these tiny immature follicles can cause the ovaries to become enlarged leading to symptoms like a heavy feeling in your abdomen or lower back pain.
These follicles are different from functional ovarian cysts, the most common type of ovarian cyst. “A functional ovarian cyst can develop for anyone (with or without PCOS) and can behave like a water balloon bursting or irritation from a slow leak," says Gouri Pimputkar, DO, clinical lead at Allara Health. The pain you’d feel from a functional cyst bursting is different from the pain you might feel from having enlarged ovaries due to PCOS.
People with PCOS are also more likely to have higher levels of inflammation and insulin resistance, both of which can cause widespread chronic pain.
Types of PCOS pain
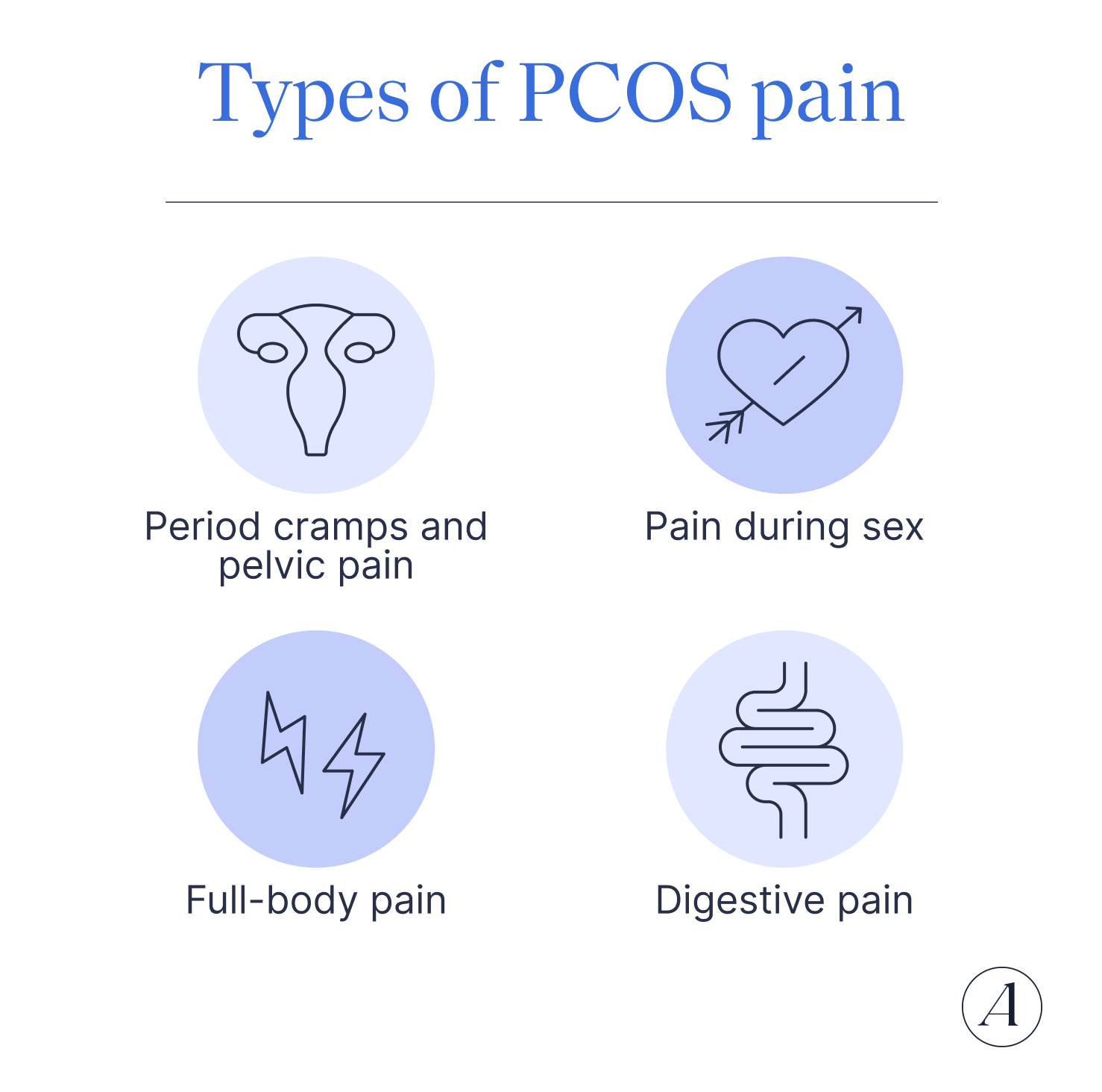
Nearly 30% of people with PCOS report experiencing pain. Beyond pelvic pain, PCOS can cause a variety of symptoms from widespread chronic pain to digestive problems. Here are some ways PCOS pain can present.
Period cramps and pelvic pain
People with PCOS regularly report experiencing cramping, bloating, and heavy bleeding. PCOS causes irregular hormone levels, which can influence your menstrual cycle. Longer menstrual cycles can lead to heavier periods.
Pain during sex
You may experience some pain during penetrative sex if your ovaries are enlarged. If you’ve been experiencing pain for a while, you may also be tightening your pelvic floor, which can lead to pelvic floor dysfunction, causing further pain.
Full-body pain
Another way PCOS causes pain is by increasing the amount of inflammation in your body. Inflammation is a natural process that helps our bodies fight off illnesses and heal from injuries. But sometimes, inflammation can occur without these triggers, leading to more harm than good. People with PCOS are more likely to have chronic low-grade inflammation. This type of inflammation can both cause widespread pain and increase your perception of pain.
Digestive pain
The inflammatory nature of PCOS can influence the bacteria in your gut. “Studies show that there might be altered gut microbial diversity with patients that have PCOS,” says Pimputkar. “The chronic inflammation of the intestinal tract also affects intestinal hormones (like GLP-1) that are important for appetite, hunger, and ultimately influence insulin resistance.” These changes to your digestive system can ultimately lead to changes in your bowel habits, nausea, and abdominal pain.
PCOS pain vs. other conditions
PCOS can co-occur with many other conditions that cause pain. Because PCOS can cause symptoms similar to other conditions, it can make it hard to tell whether your symptoms are due to PCOS or another condition. Keeping a symptom log that you can review with your healthcare provider can help you get a better sense of what’s causing your pain.
Endometriosis
Endometriosis is an inflammatory condition where tissue similar to the lining of the uterus is found outside of the uterus. Endometriosis lesions are most commonly found throughout the pelvis including on organs such as the ovaries, fallopian tubes, bladder, and colon.
It’s possible to have both PCOS and endometriosis. A small study took biopsies from 40 people with PCOS with infertility or pelvic pain and found that 76% of those studied also had endometriosis.
Endometriosis and PCOS can have similar symptoms like heavy periods, back pain, pain during sex, and digestive problems. But generally, endometriosis causes sharper cramping than PCOS. “Pain with endometriosis is typically more intense, cyclic with the menstrual cycle, significant pain with intercourse, bowel movements, or urination,” explains Pimputkar. “Pain with PCOS tends to be a heaviness, more generalized, and not specifically related to the menstrual cycle.”
Irritable Bowel Syndrome
Irritable bowel syndrome or IBS is a bowel disorder that causes abdominal pain and changes in bowel habits including diarrhea, constipation, or a combination of the two. Both PCOS and IBS can both cause changes in bowel habits, bloating, and abdominal pain.
People with PCOS are twice as likely to have IBS than those without PCOS. So far, research hasn’t proven whether one causes or increases the risk of the other. There may be several shared reasons for this connection. Hormonal fluctuations, inflammation, metabolic changes, and lifestyle and environmental factors all play a role in the development of PCOS and IBS.
Thyroid conditions
The thyroid is a small gland in the neck that secretes hormones that maintain your body’s metabolism and overall wellbeing. When your thyroid is underactive, you can experience a wide range of symptoms from fatigue, constipation, dry skin, and infrequent periods.
People with PCOS are more than twice as likely to have autoimmune thyroid disease (AITD). And AITD has been reported in up to 40% of people with PCOS. Chronic inflammation plays a significant role in both conditions -- and both can lead to metabolic issues, especially if untreated. Both PCOS and thyroid issues can cause a general sense of discomfort and a lack of wellbeing.
How to relieve PCOS pain
The best way to relieve PCOS-related pain is to address your PCOS. There are two main ways to do this: lifestyle changes and medical treatments.
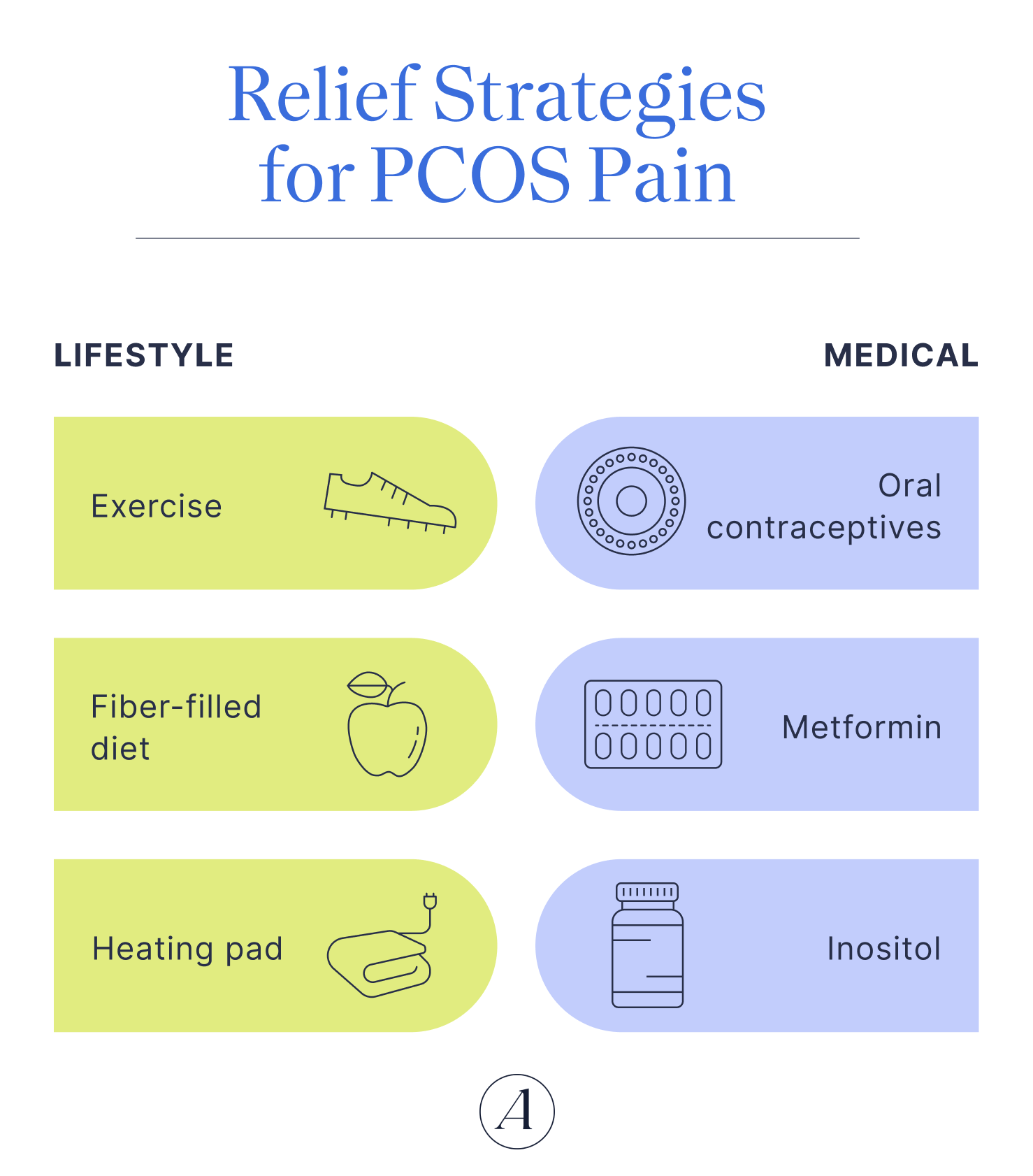
At-home and lifestyle relief
There are many at-home remedies you can try to manage your symptoms. Some of these changes can temporarily reduce pain while others may help reduce PCOS hormonal changes or insulin resistance over time.
- Stay active: Increasing physical activity can help improve insulin sensitivity and stabilize hormonal fluctuations. “This can eventually improve ovulation, reducing the pelvic pain and heaviness associated with irregular ovulation,” says Pimputkar.
- Bring on the heat: Heating pads are a great option for lower back and abdominal pain. Though heat won’t treat the problem, it can help soothe any discomfort and PCOS cramps you might be experiencing.
- Fill up on fiber: There is no one-size-fits all diet when it comes to PCOS. Still, there are a few things a PCOS-friendly diet should include namely fiber. “High fiber nutrition can help with inflammation in the intestinal tract and improve the gut bacterial environment,” says Pimputkar. Fiber can also help improve insulin sensitivity.
- Change things up in the bedroom: If penetrative sex is painful, try adding some lubrication, switching positions or other intimate acts that don’t involve insertion.
Medical Treatments
Medical treatments for PCOS pain are largely the same as the main treatments for PCOS.
- Hormonal birth control: Taking oral contraceptives can help balance hormones and shorten the length of your cycle. Improving your hormones may reduce the number of non-functional follicles, which may help reduce the amount of pain you’re experiencing.
- Metformin: Metformin is a prescription medication that can lower insulin levels and reduce insulin resistance. Reducing insulin resistance may help lower inflammation, and improve your overall wellbeing. Metformin can cause digestive upset, so it might not be a good fit if your primary symptoms are digestion related.
- Inositol: Inositol is an over-the-counter dietary supplement that can help improve insulin resistance, decrease insulin resistance, support healthy hormone function, and improve menstrual cycle regulation.
- Pelvic floor physical therapy: This can be especially helpful if you have pelvic floor dysfunction or endometriosis in addition to PCOS. A physical therapist will work with you and give you exercises to help you identify and improve muscle weakness/overactivity that may be contributing to pelvic pain.
When to see a doctor about PCOS pain
When you live with a chronic condition, it’s easy to assume that any symptoms you’re experiencing are because of that condition. Though PCOS can cause pain and discomfort, it’s important to get your symptoms, especially new ones, evaluated by your healthcare provider. Changes in your symptoms may be a sign that your treatment plan needs adjusting or be the result of a different health issue.
“I always believe that if you have concerns about pelvic pain, regardless if it is related to your cycle or not, it is important to have the conversations with your healthcare provider,” says Pimputkar.
Frequently Asked Questions (FAQs)
Is PCOS painful?
PCOS is generally not thought of as a condition that causes pain. However, many people with PCOS report experiencing pain. PCOS pain can range from widespread pain to pelvic cramping, bloating, and digestive issues.
Does PCOS cause painful periods?
Cramping is a common symptom for anyone who menstruates. Talk to your healthcare provider If your periods are regularly so painful that you find yourself avoiding work, school, or your regular routine. While PCOS can cause period pain, extremely painful periods are more often a sign of endometriosis.
Can PCOS cause back pain?
Yes, PCOS can cause back pain. Some people with PCOS tend to have larger ovaries, which can cause back pain and feelings of fullness in your pelvis.
If you have PCOS and are experiencing pain, talk to your healthcare provider. A comprehensive evaluation can help identify any underlying problems that may explain how you’re feeling. Treating insulin resistance and hormone fluctuations can make a big difference when it comes to treating PCOS symptoms, even the painful ones.
Key Takeaways
- PCOS can cause cramps, pelvic discomfort, back pain, and digestive issues — even though pain isn’t considered a main symptom.
- Enlarged ovaries and chronic inflammation can contribute to feelings of heaviness, bloating, and lower back and abdominal pain.
- PCOS can overlap with other painful conditions such as endometriosis and irritable bowel syndrome (IBS), making it harder to pinpoint the cause of pain.
- Lifestyle changes like regular exercise, a fiber-rich diet, and heat therapy can help manage discomfort. And medical options such as hormonal birth control, metformin, and inositol can address underlying hormonal and metabolic issues.
- Regular check-ins with your healthcare provider are important, since new or worsening pain may be a sign of another condition or that you need to adjust your treatment plan.











