
Low progesterone symptoms: how to know if you’re deficient
Fertility struggles, sleep issues, or irregular cycles? Those could be low progesterone symptoms, and understanding what’s behind them is essential to feeling better.
Low progesterone symptoms can feel like your body has been hijacked by hormonal chaos: irregular cycles, mood swings, headaches, spotting, sleep drama, and fertility frustrations. As someone smack in the middle of perimenopause, I know the feeling all too well (hello, insomnia and anxiety). When my provider checked my labs, they noticed my progesterone levels were dipping—a not-so-fun revelation, but one that explained a lot.
So, what’s the deal with progesterone anyway? This hormone isn’t just about pregnancy (though that’s a big part of progesterone function). It also helps regulate your cycle, supports better sleep, and even keeps your moods more stable. When levels drop, your body feels it.
Ahead, we’ll unpack what symptoms of low progesterone actually feel like, why it happens, how to test for it, and what treatments can help. Whether you’re trying to conceive, riding the rollercoaster of perimenopause, or just desperate for answers about unexplained fatigue and period changes, you’re in the right place.
What is progesterone and what does it do?
Progesterone is a steroid hormone made from cholesterol, produced mainly by the adrenal glands and ovaries. Its major job is to protect a pregnancy, says Gouri Pimputkar, DO, FACOG, DipABLM, clinical lead at Allara Health. Nicknamed the “pregnancy hormone,” progesterone preps the endometrium (uterine lining) for implantation, calms uterine contractions so pregnancy can stick, promotes gestation, and even suppresses milk production until after birth.

During the menstrual cycle, it also sparks new capillary growth, boosting blood flow and nutrient delivery. And in the cervix, it thickens mucus to block sperm and harmful microbes.
Progesterone is also “the balance to estrogen production and protects the uterus from the uterine lining becoming too thick and transforming into abnormal cells,” adds Dr. Pimputkar.
But progesterone isn’t just about reproduction. In the nervous system, it helps build myelin, the fatty sheath that protects nerve fibers. In the musculoskeletal system, it partners with estrogen to support peak bone density.
Progesterone also isn’t exclusive to those with a uterus. In people assigned male at birth (AMAB), it’s made by the testes and supports sperm development and androgen production.
In people with a uterus, progesterone levels rise and fall depending on where you are in your cycle—or whether you’re pregnant. Levels start climbing midway through the menstrual cycle, peak for about a week, then dip if no fertilization occurs. In pregnancy, they keep rising steadily. Here’s a quick look at normal ranges:
- Female (pre-ovulation): < 1 ng/mL (3.18 nmol/L)
- Female (mid-cycle): 5–20 ng/mL (15.90–63.60 nmol/L)
- Male: < 1 ng/mL (3.18 nmol/L)
- Postmenopausal: < 1 ng/mL (3.18 nmol/L)
- Pregnancy 1st trimester: 11.2–90.0 ng/mL (35.62–286.20 nmol/L)
- Pregnancy 2nd trimester: 25.6–89.4 ng/mL (81.41–284.29 nmol/L)
- Pregnancy 3rd trimester: 48–150+ ng/mL (152.64–477+ nmol/L)
Symptoms of low progesterone
Low progesterone can show up in all sorts of ways—whether it’s messing with your cycle, stirring up symptoms in pregnancy, or sparking hot flashes in perimenopause. It can even impact people assigned male at birth. Here are the most common signs of low progesterone depending on your situation.
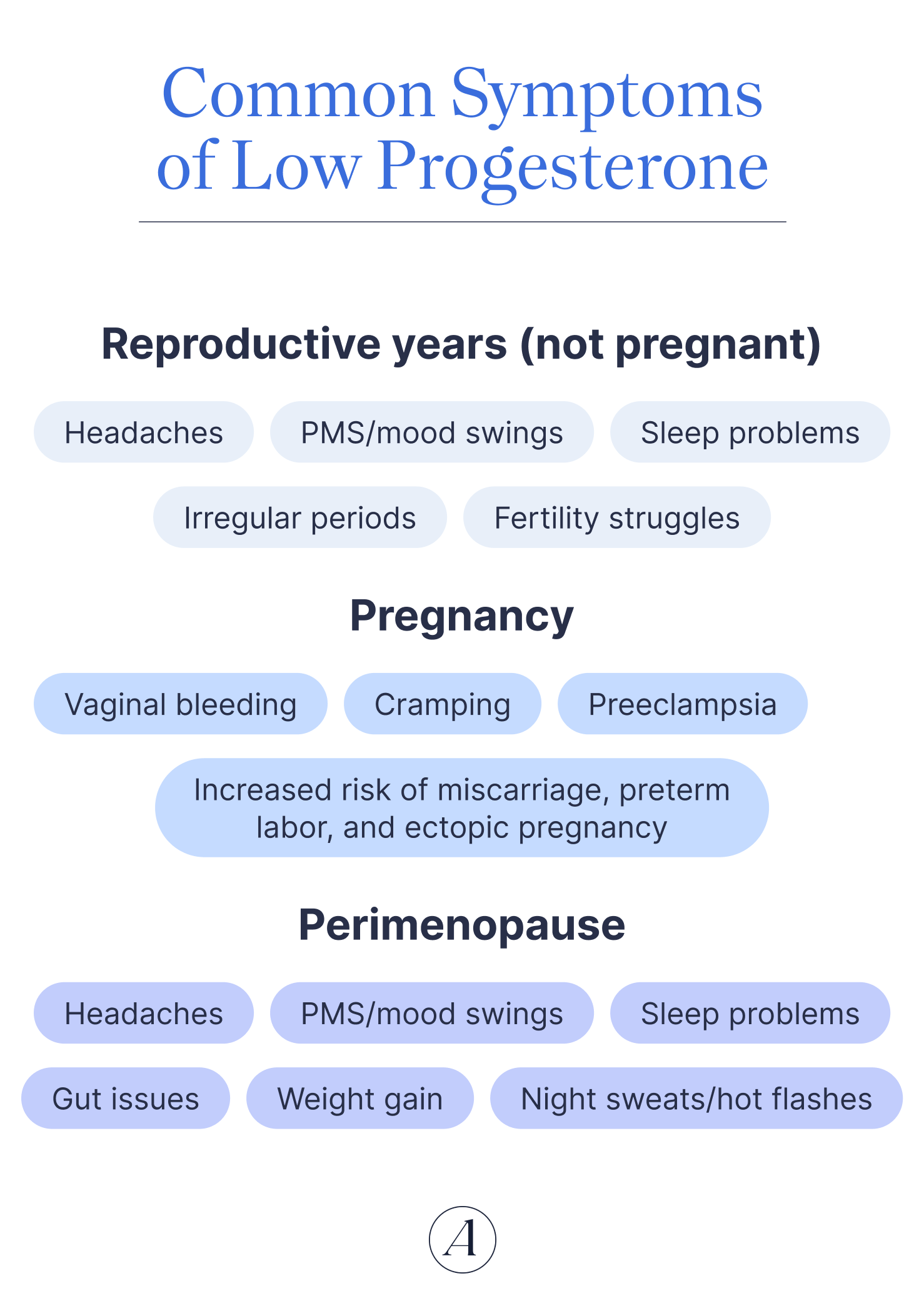
When you’re not pregnant
Headaches
Fluctuating estrogen is a well-known menstrual migraine trigger, but progesterone may play a part too. Normally, progesterone helps quiet pain signals in your brain and calm cells in your body called “mast cells”—these release histamine which can be a hallmark of allergies or itch. Progesterone can also dial down prostaglandins (hormone-like compounds) that relate to pain.
When progesterone dips, that protection may leave you more susceptible to period-triggered headaches.
PMS and mood swings
Premenstrual dysphoric disorder (PMDD)—a severe version of PMS with intense mood symptoms that occurs in the luteal phase—is linked to low (or unstable) progesterone levels.
Some research shows it’s not just progesterone levels that matter but how fast they fall. A sharp luteal-phase drop is more likely to spark those mood symptoms, while a gradual decline can keep things calmer.
Sleep problems
Progesterone has a chill, sleep-promoting effect. So when it nosedives before your period (i.e., during the late luteal phase), sleep issues often follow.
Irregular periods
Cycle all over the place? Low progesterone may be related to irregular periods. Fluctuating levels of progesterone (and estrogen) can throw off the normal rhythm of menstruation, leading to:
- Flow that’s heavier or lighter than usual
- Cycles longer than 35 days or shorter than 21
- Cycle length shifting by more than a week
- No period for months at a time
- Spotting between periods or after sex
When you are pregnant
According to Dr. Pimputkar, some signs of low progesterone levels in pregnancy include:
- Vaginal bleeding
- Abdominal pain/cramping
- An increased risk of miscarriage and pre-term labor
- Ectopic pregnancy
“Low progesterone throughout the pregnancy can also be linked to low birth weights and hypertensive problems” including preeclampsia, she adds.
When you’re perimenopausal or menopausal
Gut issues
Falling estrogen and progesterone slow down gut motility, meaning food creeps through your system at a snail’s pace. The result? Uncomfortable bathroom issues like bloating, gas, and constipation.
Weight gain
If the waistband feels tighter, hormones may be part of the story. “Typically, low progesterone is not associated with weight gain,” says Dr. Pimputkar. However, lower progesterone (and estrogen) during perimenopause and menopause can reduce muscle mass and slow metabolism, so you burn fewer calories. Add in sluggish digestion, and weight gain—especially around the midsection—becomes easier.
Hot flashes and night sweats
Vasomotor symptoms like hot flashes and night sweats are super common (8 out of 10 perimenopausal people experience them). Fluctuating estrogen and progesterone are big culprits of these sweaty symptoms. Some research suggests micronized oral progesterone can help take the edge off those sweaty nights.
Sleep sabotage
Progesterone usually promotes better zzz’s, but its decline in perimenopause often does the opposite. No wonder 51.6% of postmenopausal people report sleep problems. Hormone therapy (often with estrogen and progesterone) can sometimes bring big improvements here.
Mood swings
During the reproductive years, lower progesterone is linked to PMDD and mood symptoms, and it can still impact mood later in life. In perimenopause, drops in progesterone can stir up mood swings and even worsen psychosomatic conditions like irritable bowel syndrome.
Around 35% of menopausal people worldwide report depression. Some research also shows anxiety is common as well, with an estimated 52.5% of menopausal people and 55.7% of perimenopausal people experiencing symptoms.
Headaches
Perimenopause can feel like a hormonal rollercoaster with constantly fluctuating estrogen and progesterone. These rapidly changing levels can trigger symptoms like headaches during perimenopause.
When you’re AMAB
“Progesterone levels in males can impact sperm production and function,” says Dr. Pimputkar. So when levels are low, they may be associated with:
- Lower testosterone levels
- Sexual dysfunction
Causes of low progesterone
From skipped ovulation to stress overload, there are many possible causes of low progesterone.
Anovulation
Anovulation—when your ovaries don’t release an egg—can tank progesterone. In these anovulatory cycles, estrogen is still produced, but without ovulation there’s no corpus luteum (the structure that normally pumps out progesterone). One study even found that people with a single anovulatory cycle tended to have lower progesterone levels.
PCOS
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in people with a uterus of reproductive age—affecting about 1 in 5. It’s marked by hormonal dysregulation, including frequent anovulatory or irregular ovulatory cycles. The result? Lower progesterone is common for many with PCOS.
Hyperprolactinemia
Prolactin is the hormone that helps with milk production and breast development, but too much of it (a condition called hyperprolactinemia) can inhibit ovulation. High prolactin levels block gonadotropin releasing hormone (GnRH) which can ultimately influence the production of follicle stimulating hormone (FSH)—a key hormone needed for follicular development. No ovulation means no progesterone surge.
Thyroid problems
Your thyroid—the tiny, butterfly-shaped gland in your neck—helps regulate reproductive balance in people with a uterus. Thyroid hormones play a role in protein messengers "talking" with certain cells in your ovary that are responsible for progesterone production. Sometimes, this can trigger hyperprolactinemia, which can further disturb hormone production, but that isn't the only “why” as to how this occurs. Hypo- and hyperthyroidism—whhen the thyroid is underactive or overactive, respectively—can both cause changes to cycles. Fewer ovulatory cycles = lower progesterone.
Menopause
Progesterone naturally declines during the menopause transition, eventually reaching very low levels. For context: postmenopausal levels hover under 0.5 ng/ml, compared to 5–20 ng/ml during the luteal phase of a typical menstrual cycle.
Stress
Chronic stress can affect the brain-to-ovary messaging system that controls ovulation and progesterone production, says Dr. Pimputkar. As she explains, this can lead to irregular cycles, irregular ovulation, infertility, and even a higher risk of pregnancy loss.
Lifestyle habits
Too much exercise or too little food can send your body into “survival mode.” “Similar to high stress and a dysregulated cortisol response, over-exercising and excessive restriction of food tell the brain and body it’s not safe to ovulate,” says Dr. Pimputkar. “That sets off a cascade of events which will eventually lead to low progesterone levels and irregular or absent periods.”
How low progesterone affects fertility and pregnancy
Progesterone is essential for a healthy pregnancy. One of its main jobs is to stop the uterine muscle (the myometrium) from contracting too much, which helps implantation go smoothly and prevents the body from accidentally expelling the pregnancy too soon.
Progesterone also regulates the production of immune cells like T-cells in the uterine cavity. Without enough of it, immune defenses weaken.
Coupled together, these effects of low progesterone can raise the risk of miscarriage, early delivery, or other pregnancy complications. Low progesterone has even been tied to low birth weight and high blood pressure during pregnancy, notes Dr Pimputkar.
Low progesterone in women doesn’t just cause issues once you’re pregnant—it can also make it harder to get there in the first place. During the second half of the menstrual cycle, progesterone thickens and primes the uterine lining, creating a plush landing pad for a fertilized egg. If levels fall short, the endometrium may not be prepared for implantation, possibly lowering the odds of a successful pregnancy.
How to test for low progesterone
If your body’s sending up red flags—like irregular cycles, fertility struggles, or pregnancy issues—your provider may order a blood test to measure progesterone. This is the gold standard for spotting whether low levels are part of the problem.
Levels naturally rise and fall depending on where you are in your cycle, whether you’re pregnant, or if you’re postmenopausal. Here’s a quick cheat sheet of what “normal progesterone levels” looks like:
- Female (pre-ovulation): < 1 ng/mL (3.18 nmol/L)
- Female (mid-cycle): 5–20 ng/mL (15.90–63.60 nmol/L)
- Male: < 1 ng/mL (3.18 nmol/L)
- Postmenopausal: < 1 ng/mL (3.18 nmol/L)
- Pregnancy (1st trimester): 11.2–90.0 ng/mL (35.62–286.20 nmol/L)
- Pregnancy (2nd trimester): 25.6–89.4 ng/mL (81.41–284.29 nmol/L)
- Pregnancy (3rd trimester): 48–150+ ng/mL (152.64–477+ nmol/L)
That said, one blood test may not tell the full story. Because progesterone levels during your cycle can fluctuate throughout the month (or even day-to-day), your provider may want multiple blood draws to really see what’s going on.
Additionally, urine tests for PDG (a progesterone metabolite) are now available as home test strips. Handy, yes—but not foolproof. Since hormone levels shift so much, it’s still best to bring your results (and questions) to your provider for proper interpretation.
Treatments for low progesterone
If low progesterone is secondary to another issue—like thyroid problems, PCOS, or high prolactin—the first step is treating that root cause. Often, once the underlying condition is managed, hormone levels may start to balance out naturally.
When symptoms stick around, medical treatments for low progesterone can help. Progesterone comes in two main types: natural (often derived from plants) and synthetic (called progestins). You’ll find it as pills, vaginal inserts, or injections, depending on what your body needs.
Here are a few ways progesterone therapy can help:
- Progestins (alone or in combo formulas) can ease painful periods, irregular cycles, abnormal bleeding, or endometriosis-related pain.
- When paired with estrogen, progestin-containing contraceptives can treat conditions like PCOS-related oligomenorrhea, menstrual migraines, PMS, or PMDD.
- For those with a uterus, progestins are combined with estrogen in hormone replacement therapy (HRT) to reduce hot flashes and other vasomotor symptoms in menopause.
- Oral micronized progesterone can also improve sleep and cut down night sweats in perimenopause.
- Progesterone therapy is used to lower the risk of miscarriage (especially with early bleeding and recurrent losses) and to prevent preterm labor.
- Micronized progesterone, progesterone in oil intramuscular injection, or vaginal micronized progesterone is also a standard part of IVF protocols, supporting the uterus after embryo transfer.
Keep in mind: The type of progesterone—and how it’s delivered—depends on your health history and goals. That’s why it’s key to work with a healthcare professional to find the right fit for you.
Natural ways to support progesterone
If you’d rather explore non-medical ways to increase progesterone, lifestyle shifts and holistic approaches can make a real difference.

Stress management
Chronic stress can sabotage progesterone (during stressful times, your body may even convert progesterone to cortisol, your main stress hormone).
Mindfulness, cognitive behavioral therapy, relaxation training, or even a good meditation app can all help calm your system and protect those hormone levels, says Dr Pimputkar.
Sleep
Good sleep habits (a.k.a. sleep hygiene) help regulate your circadian rhythm and restore insulin function, especially key for people with PCOS, says Dr. Pimputkar. Translation: prioritizing sleep isn’t just about feeling rested, it’s about giving your hormones the reset they need.
Move your body
Exercise can lower cortisol and improve sleep, both of which support healthy hormones. The catch? Overtraining does the opposite, stressing your body into thinking it’s not safe to ovulate, says Dr. Pimputkar. Gentle options like yoga—which is known to reduce cortisol—strike the right balance.
Acupuncture
Early research suggests acupuncture may help nudge up progesterone levels, but the evidence isn’t conclusive yet. Still, many people find it a relaxing and supportive part of their routine.
Nutrient-dense diet
A balanced diet fuels hormone production and overall reproductive health. Think colorful fruit and veggies, whole grains, lean proteins, and healthy fats. Bonus tip: ascorbic acid (vitamin C) has been linked with higher progesterone levels, so fill your plate with plants like kiwi, peppers, and oranges.
Supplements
The right supplements can support ovulation (and by extension, progesterone production), says Dr. Pimputkar. “Myo-Inositol and Vitamin D have been shown to restore ovulation, especially in women with PCOS or insulin resistance, [while] folate, CoQ10, and omega-3 fatty acids can also help improve ovarian function,” she says.
When to see a doctor
Yes, progesterone naturally dips with age, but that doesn’t mean you need to white-knuckle your way through hot flashes, sleepless nights, or mood swings. If symptoms are stealing your quality of life, it’s worth checking in with a professional. And if you’re still years away from perimenopause or your symptoms feel especially intense, that’s an even louder signal something deeper might be at play.
Sometimes your body throws up signs that deserve more than a shrug. Call your doctor if you:
- Struggle to get pregnant
- Have abnormal bleeding when you’re not pregnant
- Experience irregular periods, hot flashes, sleep issues, mood changes, or migraines
- Notice cramps or bleeding that could point to a miscarriage or ectopic pregnancy
You don’t have to grin and bear it. Clinical experts—like the team at Allara—can help get to the root of what’s going on, guide you through treatment options, and support you every step of the way.
Bottom line
Low progesterone isn’t just a hormone hiccup. It can ripple through your mood, cycles, fertility, and overall wellbeing. With the right testing, treatment, and lifestyle tweaks, balance is possible.
If you’re dealing with stubborn symptoms, you don’t have to tough it out. The experts at Allara can dig deep, diagnose what’s really going on, and create a plan to get your hormones back on track, so you can feel in sync with your body again.
Key takeaways
- Progesterone plays a starring role in fertility, pregnancy, sleep, mood, and cycle regulation.
- Low progesterone can trigger symptoms like irregular periods, migraines, mood swings, sleep issues, and even infertility issues.
- Causes range from PCOS, thyroid disorders, and stress to menopause and lifestyle factors.
- Testing is key since progesterone levels naturally rise and fall with your cycle (and pregnancy).
- Treatment may include medical therapy, hormone support, or lifestyle shifts—what’s best depends on your body and needs.
Frequently asked questions (FAQs)
Can progesterone make you drowsy?
Yep, it can. Some oral forms of progesterone come with side effects like drowsiness, dizziness, or headaches. If you notice these, let your provider know. They may be able to tweak your dose or switch you to a different type.
What does progesterone do?
Progesterone’s main function is to prepare the body for pregnancy. In the second half of your cycle, once an egg is released, progesterone levels rise to get your uterus ready. If pregnancy happens, levels keep climbing to maintain it. High progesterone levels:
- Help the uterine lining produce proteins that support implantation.
- Make white blood cells that stop your immune system from rejecting the embryo.
- Keep the uterus calm and relaxed (no early contractions).
- Support placenta development, so the fetus gets the oxygen and nutrients it needs.
Can you get pregnant with low progesterone?
It’s trickier. Progesterone primes the uterine lining for implantation. If levels are too low, the endometrium may not be ready, which can lower your chances of conceiving or carrying to term.
Can low progesterone cause anxiety?
It might. Low progesterone is tied to mood symptoms, including PMDD during reproductive years. In perimenopause, dropping levels can also bring mood swings. Research shows anxiety is common, affecting about 55.7% of people going through perimenopause and 52.5% those in menopause.












