
If you’re feeling anxious, constantly tired, or are struggling with digestive issues but can’t pinpoint the exact cause, too much cortisol may be to blame. While these are all signs of high cortisol, they are also possible symptoms of many other health conditions. Here’s how to figure out what’s going on and when to see a doctor.
Cortisol is confusing, mainly thanks to the misinformation spread online about this hormone. If you’re chronically on TikTok or Instagram like me, you’ve probably seen videos talking about the signs of high cortisol or how to lower cortisol levels, mainly through stressing less. While most of us could probably benefit from better stress management (myself included), this isn’t the whole story behind cortisol.
For one thing, cortisol is something our bodies need, and which fills many roles for our health. Plus, truly having too much cortisol is more than just being stressed. To get a more accurate picture of the “stress hormone,” we have to understand how cortisol works (spoiler alert: this hormone’s effects aren’t all negative, and they extend well beyond emotional stress), as well as possible high cortisol symptoms.
What is cortisol?
Cortisol is often pigeon-holed as the “stress hormone,” when in reality, this hormone is responsible for a lot more. It plays a role in regulating your immune system, mood, metabolism, blood sugar, and blood pressure. The adrenal glands, small glands at the top of the kidney, make and release cortisol, alongside other steroids, adrenaline, and noradrenaline.
But the adrenal glands don’t work alone. And buckle up, because we’re about to revisit anatomy 101. The process to make cortisol starts in the hypothalamus, the region of the brain that coordinates the endocrine system (organs involved in hormone production). When the hypothalamus releases corticotrophin-releasing hormone (CRH), CRH then triggers the anterior pituitary gland, a small gland in the brain that produces essential hormone, to release adrenocorticotropic hormone (ACTH). ACTH then communicates to the adrenal gland that it should create and release cortisol.
This entire process needs something to trigger it, which is where stress comes in. When we’re stressed, the hypothalamus responds by producing more CRH—and this is actually what it’s designed to do. “Cortisol is our fight-or-flight hormone, so it's supposed to rise in situations of physical or emotional stress,” says Sonia Gibson, MD, a lead Board Certified Endocrinology Physician at Allara.
Stress, however, isn’t the only trigger. The release of cortisol can be part of the inflammatory response to an illness or injury, part of the body’s response to eating, or a reaction to spikes in blood sugar (which can be due to various causes from eating foods high in sugar to skipping breakfast to sunburn), among other triggers.
Cortisol is also released in varying amounts throughout the day as part of the 24 hour Circadian rhythm. Your body naturally releases more cortisol in the morning to help wake up, and levels drop when it’s time to sleep.
But too much of anything, including cortisol, can lead to issues. While cortisol spikes and dips naturally throughout the day, excess cortisol can lead to negative impacts on health (which we’ll go into below).
Pathological high cortisol “is a state of cortisol oversecretion for a prolonged period, either due to an adrenal or pituitary tumor, or prolonged exogenous corticosteroid use,” says Dr. Gibson. When a tumor or the use of corticosteroid medications is to blame, someone may be diagnosed with Cushing’s Syndrome, a rare condition where the body produces too much cortisol.
High levels of stress cannot cause Cushing’s Syndrome, though physical or emotional stress may lead to transient periods of high cortisol, which is sometimes referred to as pseudo-Cushing’s syndrome. Causes of pseudo-Cushing’s include severe depression, alcoholism, poorly controlled diabetes, obesity, eating disorders, or critical illness.
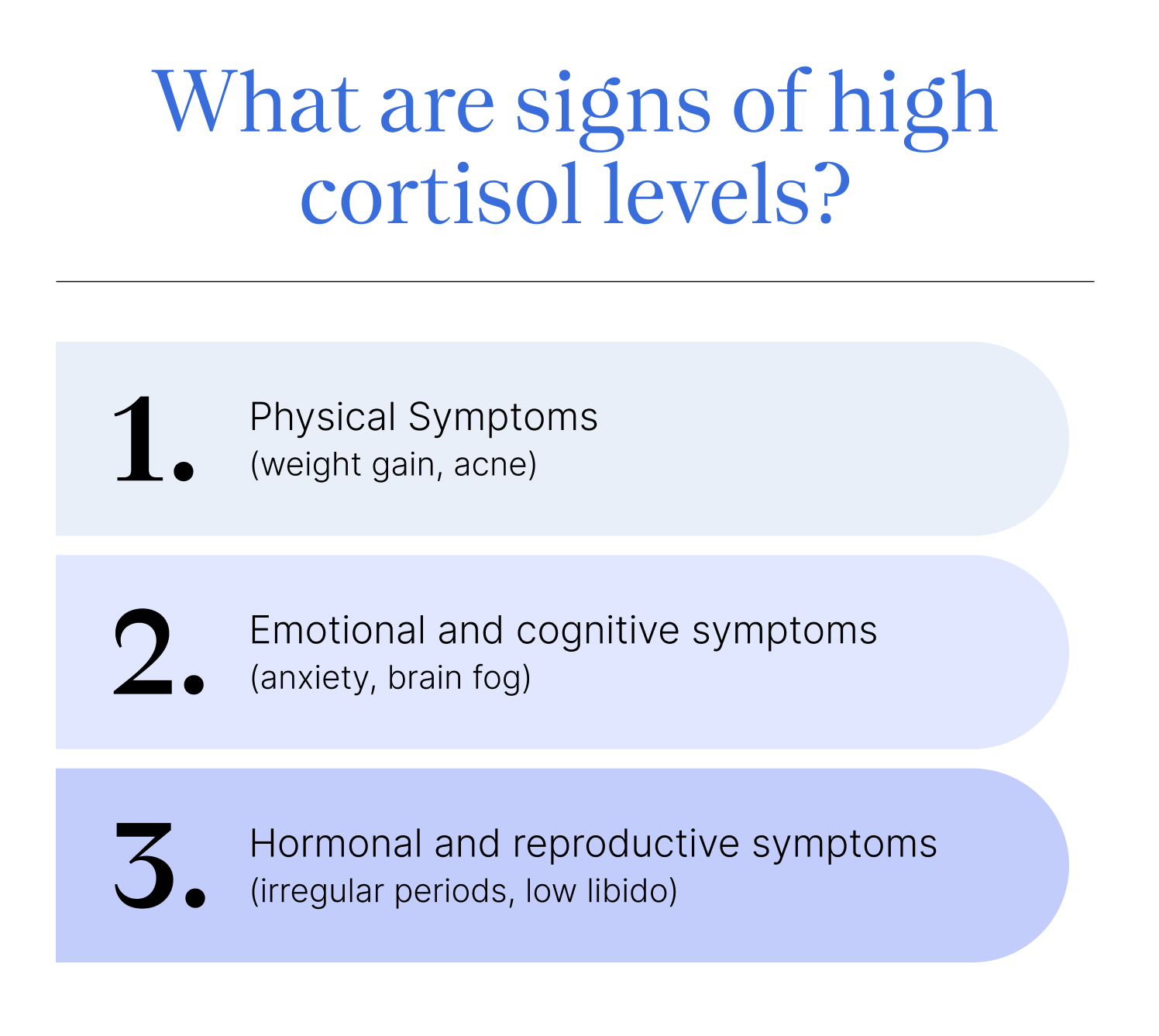
What are signs of high cortisol levels?
If we all experience cortisol spikes throughout the day, how can you tell when there’s too much cortisol? High cortisol often manifests as physical, emotional, and hormonal symptoms, such as the signs listed below.
As you continue reading, remember that high cortisol impacts everyone differently. If you have high cortisol, you probably won’t experience all these symptoms.
Physical Symptoms
As we’ve established, cortisol plays a role in many, many systems in the body. When cortisol levels are abnormally elevated or pathologically high, it disrupts the immune system, our sleep-awake cycle, metabolism, digestion, and the body’s ability to regulate blood sugar and blood pressure.
Physical symptoms include:
- Weight gain, especially around the waist which is sometimes referred to as cortisol belly
- Acne
- High blood pressure
- Headaches
- Gastrointestinal symptoms like abdominal pain, constipation, or diarrhea
- Increased thirst
- Disrupted sleep, including insomnia
Emotional and Cognitive Symptoms
When cortisol levels increase, activity decreases in the prefrontal cortex, the part of the brain responsible for executive functions like planning and problem solving. Activity increases in the amygdala, the part of the brain responsible for storing your emotional memory and regulating emotions like fear and anxiety. This means that when cortisol is high, we react more emotionally and have lower levels of self-control and cognitive flexibility, which is the ability to adapt to new situations or circumstances.
If stress and cortisol levels remain high, this can have a long term impact on mental and cognitive health, causing symptoms such as:
- Anxiety
- Brain fog or trouble concentrating
- Depression
- Fatigue
- Irritability
In severe cases, excess stress and cortisol are associated with the progression of Alzheimer’s disease.
Hormonal and Reproductive Symptoms
The endocrine system is made up of team players, meaning if one hormone or organ in the system is off, it may cause a ripple effect. Cortisol plays a role in that system, and when there is excess cortisol, other processes carried out by the endocrine system are disrupted too, including the menstrual cycle and female fertility. This could result in symptoms such as irregular periods, higher likelihood of being infertile, and a low libido.
It’s important to note, however, that research on cortisol’s impact on the reproductive system is still emerging. Cortisol and infertility in particular have a complicated relationship, and there are many other hormonal disruptions that are more likely to cause infertility than excess cortisol.
Serious Signs Linked to Cushing’s Syndrome
Those with Cushing’s Syndrome can experience all the symptoms listed above, as well as additional long-term symptoms like:
- Moon face, which is a red, puffy face
- Buffalo hump, which is excess fat at the base of the neck
- Weak muscles
- Purple stretch marks
- Easy bruising
- Wide purple stretch marks, often around the abdomen, hips, underarms, or breasts
- A lack of periods
- Hirsutism, excessive hair growth, specifically in those assigned female at birth
Cushing’s Syndrome also increases the risk of osteoporosis, a condition where bones become weak and brittle, because cortisol plays a role in bone development (seriously, what is cortisol not involved with?).
Since cortisol also plays a role in the immune system and inflammation levels in the body, Cushing’s is tied to a higher risk of diabetes, cognitive impairment, and atherosclerosis, a condition where the arteries become narrowed and there’s a higher risk of a heart attack or stroke.
How is high cortisol diagnosed?
When reading that list of symptoms, you may have noticed it’s pretty nonspecific. Fatigue could stem from depression or an autoimmune disease as well, GI symptoms from irritable bowel syndrome (IBS) or Crohn’s disease, and irregular periods from PCOS or endometriosis. In fact, almost every symptom listed could be attributed to at least one other condition. This is part of the reason why it’s hard to diagnose high cortisol.
“Most people misattribute symptoms like weight gain and ‘cortisol belly and face’ to excess cortisol. While these can be due to a pathological cause, Cushing's disease is rare,” says Dr. Gibson, “There are many other causes for these symptoms that have nothing to do with cortisol.”
The only way to tell if nondescript symptoms are related to elevated cortisol levels is to consult a trained healthcare provider, usually an endocrinologist. They can assess symptoms and, when necessary, order hormone tests.
“There are three diagnostic tests that can be used: saliva, urine, and blood. These are not simple tests and involve specific protocols,” says Dr. Gibson. Since cortisol levels vary throughout the day, multiple samples often need to be taken, usually at different times of the day. Your doctor may also tell you to rest and not do anything physically or emotionally intense the day before, since exercise and stress can increase cortisol levels.
What causes high cortisol levels?
If cortisol test results come back and levels are high, your doctor will probably order more tests to figure out the exact cause. Potential causes of high cortisol levels include:
- Taking high doses of medications with steroids. These medications may be prescribed to manage conditions like lupus, rheumatoid arthritis, and asthma.
- A tumor in the pituitary gland that’s causing an overproduction of ACTH, the hormone that tells the adrenal gland to make cortisol.
- A tumor in the adrenal glands that’s leading to the overproduction of cortisol.
Emotional and physical stress may also cause transient high cortisol levels, which can show up in tests. That’s why doctors often ask people to rest the day before a cortisol test and won’t order the test when you’re injured or ill.
Physical stressors range from illness and injury to intense exercise or extreme weather. Emotional stressors could be due to the loss of a loved one, a major move, or a change in employment or financial status, as well as smaller stressors, like a traffic jam or social media overload.
Not all stressors are bad or likely to lead to long-term elevation of cortisol levels. Acute stressors are a short-term response to a stressful situation, such as a big presentation at work or a hard workout. Chronic stressors, like being stuck in a high-pressure job or having a chronic illness, persist over an extended period.
And even though we sound like a broken record, it’s worth repeating: stress won’t cause Cushing’s syndrome.
How is high cortisol treated?
“Treatment depends on the cause,” says Dr. Gibson, “If it's due to adrenal or pituitary tumors, surgery may be the primary treatment, but medications might also be needed in addition to surgery. If the cause is prolonged corticosteroid use, then a slow weaning of these drugs would be necessary to allow the body to regulate cortisol on its own again.”
For high cortisol without the presence of Cushing’s syndrome, there isn't one set treatment. Instead, a doctor will identify the underlying reason why cortisol levels are so high, such as a chronic illness or ongoing emotional stress, and help create a treatment plan.

When emotional stress is to blame, a doctor may refer you to a licensed mental health provider for treatment, as well as provide some lifestyle changes to lower stress levels, such as:
- Meditation
- Breathwork
- Journaling
- Spending more time relaxing or engaged in hobbies
- Practicing daily gratitude
- Eating a well balanced diet
- Getting enough sleep
- Limiting alcohol
While stress management can help when cortisol is high due to chronic stress, the above are not treatment options for Cushing’s syndrome.
Key takeaways
- Signs of high cortisol include physical symptoms like acne and abdominal pain, emotional symptoms such as anxiety and irritability, and hormonal symptoms like missed periods.
- Since many symptoms of high cortisol could be attributed to other causes, a qualified medical professional, such as an endocrinologist, must test cortisol levels. After establishing that cortisol levels are high, they’ll determine if it’s Cushing’s Syndrome or pseudo-Cushing’s Syndrome.
- Cushing’s Syndrome treatment may include adding or slowly weaning off medications or surgery to remove tumors.
- Reducing emotional stress won’t treat Cushing’s Syndrome, though it may address high cortisol levels that aren’t associated with this medical condition.
- If experiencing any of the signs of high cortisol, the team at Allara Health can help you determine if high cortisol or something else is causing symptoms and create a customized treatment plan.
Frequently Asked Questions (FAQs)
How do I tell if my cortisol level is high?
The only way to tell for sure if cortisol levels are high is to take a cortisol test. This test measures the level of cortisol in either your blood, saliva, or urine. That said, there are very specific protocols for these tests, making it important to work with a healthcare provider.
Can high cortisol cause headaches?
When cortisol levels are high for extended periods of time, it may sometimes cause headaches. However, headaches are more likely to occur from chronic stress and they are a less common symptom of Cushing’s syndrome, which is when cortisol levels are high due to a tumor or extended use of steroid medications.
What does high cortisol feel like?
High cortisol may feel different for everyone. Many people experience emotional symptoms like anxiety, feeling wired or on edge, or irritability. High cortisol may also lead to brain fog or difficulty concentrating.
Where is cortisol produced?
Cortisol is produced in the adrenal glands, two small glands that sit at the top of the kidneys and produce multiple hormones, including cortisol.
Is “moon face” always caused by cortisol?
Moon face, a puffy or swollen face, can be caused by Cushing’s syndrome, a rare condition where the body overproduces cortisol. This isn’t the only cause of moon face. More common ones include an unbalanced diet, lack of sleep, or even sleeping with pressure placed on the face.












