
Is your period suddenly shorter, heavier, missing, or doing…seemingly whatever it wants? Perimenopause periods can be confusing, unpredictable, and totally unsettling, but once you understand what’s driving the changes, it gets a lot easier to know what’s normal, what’s not, and when to get support.
Do perimenopause periods have you scratching your head? One month your periods are getting closer together, the next they’re late, heavy, light, fast and furious, or dragging on forever—and suddenly you’re Googling long periods during perimenopause at 2 a.m., wondering if this is normal or a red flag.
If this feels personal, I’m right there with you. As someone in the thick of perimenopause myself, I’ve been navigating the stormy seas of period upheaval after decades of clockwork cycles. It’s disorienting. Confusing. Some months, even a full-on hormonal rollercoaster.
And yet, many people are brushed off with a vague “it’s probably hormones,” without anyone explaining which hormones, why they’re misbehaving, or when perimenopause period changes deserve a closer look. This article is here to change that. We’ll break down what’s actually happening in the perimenopause menstrual cycle, the most common bleeding patterns, what’s considered normal (even if it’s annoying), and when it’s time to check in with a doctor—so you can feel informed, validated, and a whole lot less in the dark.
How perimenopause affects your period
Perimenopause—literally meaning “around menopause”—is the transition leading up to your final period. It typically begins in your mid- to late 40s and lasts about four years on average, though for some people it can stretch longer or shorter.
Period quality and timing can be all over the place during perimenopause, says Gouri Pimputkar, DO, FACOG, DipABLM, clinical lead at Allara Health. Periods may come sooner—showing up as more frequent periods—or arrive late, be heavier or lighter than usual, or include unexpected spotting. “All of these changes are reflective of the ovary working really hard to ovulate as the follicle egg supply is starting to diminish,” Dr. Pimputkar explains.
For reference, “we have approximately 2 million eggs” at birth and “by the time we reach the age of 40, we have approximately only 3% left,” says Dr. Pimputkar.
This declining ovarian reserve also drives hormonal fluctuations in perimenopause, says Dr. Pimputkar. Estrogen levels can spike and dip unpredictably. Progesterone, which works closely with estrogen to regulate ovulation and your menstrual cycle, also becomes erratic.
Hormones tied to follicles shift too: follicle-stimulating hormone (FSH) rises, while inhibin B and anti-Müllerian hormone (AMH) drop. These changes can start up to a decade before menopause, often without obvious symptoms, but they’re part of why cycles become less reliable over time.
Together, all these hormonal swings can throw off ovulation, leading to periods that arrive early, late, heavier, lighter—or not at all. In fact, irregular periods are often the earliest sign that perimenopause has begun, says Dr. Pimputkar.
Common perimenopause period patterns (and what they mean)
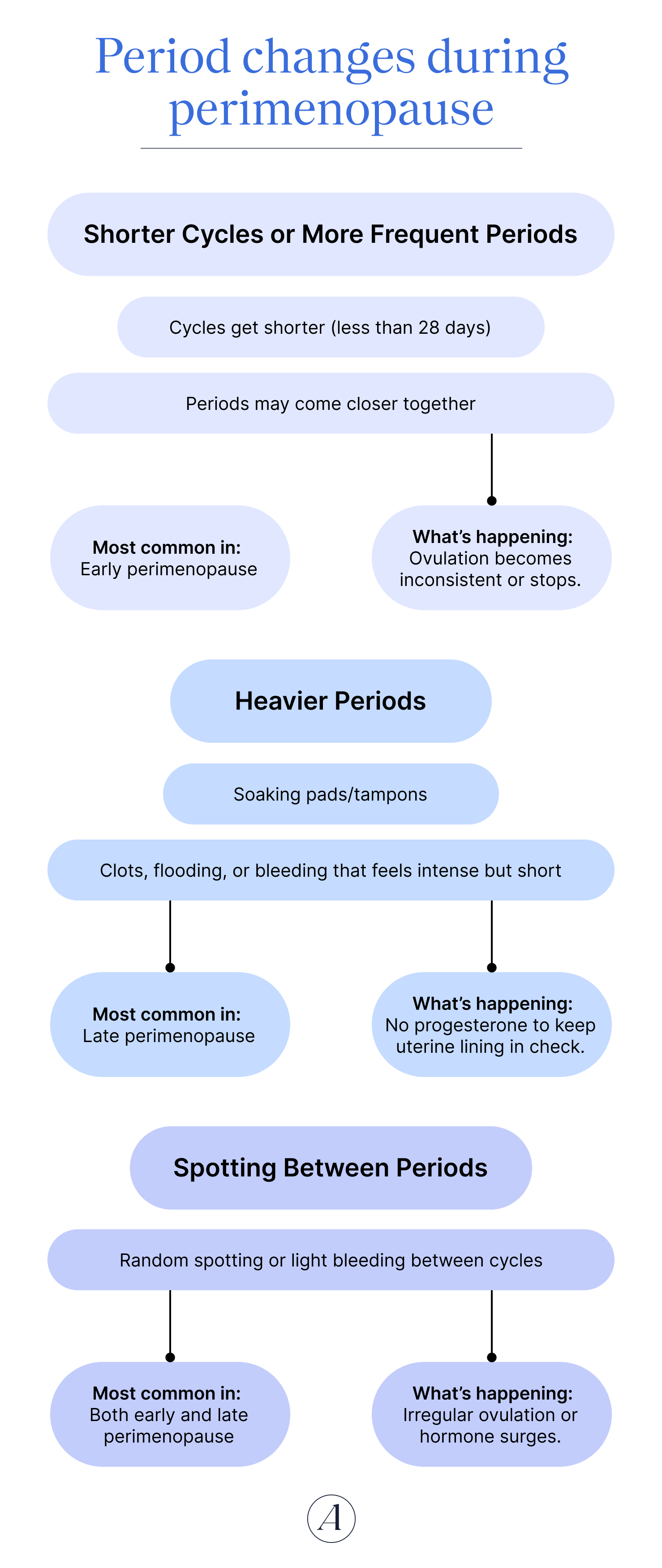
Shorter Cycles or More Frequent Periods
- Cycles get shorter (less than 28 days)
- Periods may come closer together
Most common in: Early perimenopause
What’s happening: Estrogen surges earlier in the cycle, triggering ovulation sooner—or trying to.
Longer Cycles or Skipped Periods
- Cycles stretch beyond 35–60 days
- You may skip a month (or a few) entirely
Most common in: Late perimenopause
What’s happening: Ovulation becomes inconsistent or stops some months, so progesterone doesn’t rise to trigger a period.
Heavier Periods
- Soaking pads/tampons
- Clots, flooding, or bleeding that feels intense but short
Most common in: Late perimenopause
What’s happening: Estrogen builds the uterine lining, but without ovulation, there’s no progesterone to keep it in check.
Spotting Between Periods
- Random spotting or light bleeding between cycles
Most common in: Both early and late perimenopause
What’s happening: Irregular ovulation or “out-of-sync” hormone surges (including LOOP cycles).
If your period feels like it’s making up new rules, welcome to perimenopause. While every menopausal transition is different, certain period patterns show up again and again during perimenopause. That said, not everyone notices changes—about 15–25% of people experience little to no shift in cycle regularity before menopause. Still, if things do change, here’s what’s most common—and why.
Shorter or longer cycles
Cycle changes are often one of the earliest signs of perimenopause, but how they change depends on where you are in the transition.
In early perimenopause, cycles often get shorter. As egg follicles decline, “the body attempts to compensate” by shortening the follicular phase—the time between your period and ovulation, says Dr. Pimputkar. “Estrogen levels may spike or surge earlier in the cycle, triggering premature ovulation and thus a shorter cycle overall,” she explains.
Later on, the opposite tends to happen. As menopause approaches, cycles often grow longer. “The later phase of perimenopause is characterized by spaced out periods, usually greater than 60 days apart,” says Dr. Pimputkar. Why? The ovaries struggle to produce enough estrogen to support ovulation. “Without ovulation, the body doesn't produce the necessary rise in progesterone in the latter half of the cycle, which is what normally triggers a period,” she explains. The result: very long, unpredictable cycles and late perimenopause periods.
Skipped periods or months without bleeding
Skipped periods—or stretches of no bleeding at all (amenorrhea)—are a classic sign of the menopausal transition and are closely tied to the same hormone shifts that cause longer cycles.
As ovarian function declines, the follicular phase can stall or fail altogether, says Dr. Pimputkar. In plain terms: the ovary may not make enough estrogen to trigger ovulation. No ovulation means no progesterone rise, and, without that, the uterus doesn’t get the signal to shed its lining, she explains. The result? Sometimes a completely missed period.
Heavier (or lighter) periods
Another hallmark of the menopausal transition is a change in how much (and how long) you bleed. Many people experience heavier and longer periods, especially in late perimenopause. Research shows menstrual blood loss increases with age, with women nearing their final menstrual period experiencing the heaviest bleeding.
Sometimes, heavier periods are linked to anovulation. When ovulation doesn’t occur, estrogen can act without progesterone to balance it, says Dr. Pimputkar. This can cause long cycles or skipped periods. However, “when bleeding finally does occur, it's often heavier because the uterine lining has built up unchecked due to unopposed estrogen,” she explains.
Heavy bleeding tends to be more common in people with obesity or uterine fibroids (leiomyomas), but it can happen to anyone during perimenopause.
On the flip side, hormonal swings can also produce lighter-than-usual periods or shorter periods, says Dr. Pimputkar.
Important note: While heavier periods are common during perimenopause, very heavy bleeding (known as menorrhagia)—think: periods that last more than 7 days or interfere with daily life—is not considered normal and should always be discussed with a healthcare provider.
Bleeding between periods or spotting
Spotting during perimenopause is another frequent pattern, and the numbers back that up. In one study, 66.8% of people had at least three episodes of spotting lasting six days or longer (51.2% experienced this pattern in early perimenopause, and it jumped to 75.2% in late perimenopause).
Bleeding between periods can occur when ovulation is irregular or absent (which often happens in perimenopause). But it can also signal other conditions, including, in rare cases, cancer. That’s why any bleeding between periods during perimenopause should be evaluated, even if it seems minor.
Luteal-out-of-phase (LOOP) cycles
Luteal-out-of-phase (LOOP) cycles are unique to the menopausal transition and can explain a lot of perimenopausal chaos. They occur when a second, premature wave of follicle growth pops up after ovulation, during the luteal phase.
This triggers another estrogen surge when progesterone should be in charge—throwing everything off balance. The result can be high estradiol, low progesterone, and sometimes heavy bleeding. In short: hormonal overlap, mixed signals, and a very confused uterus.
What’s normal during perimenopause — and what’s not
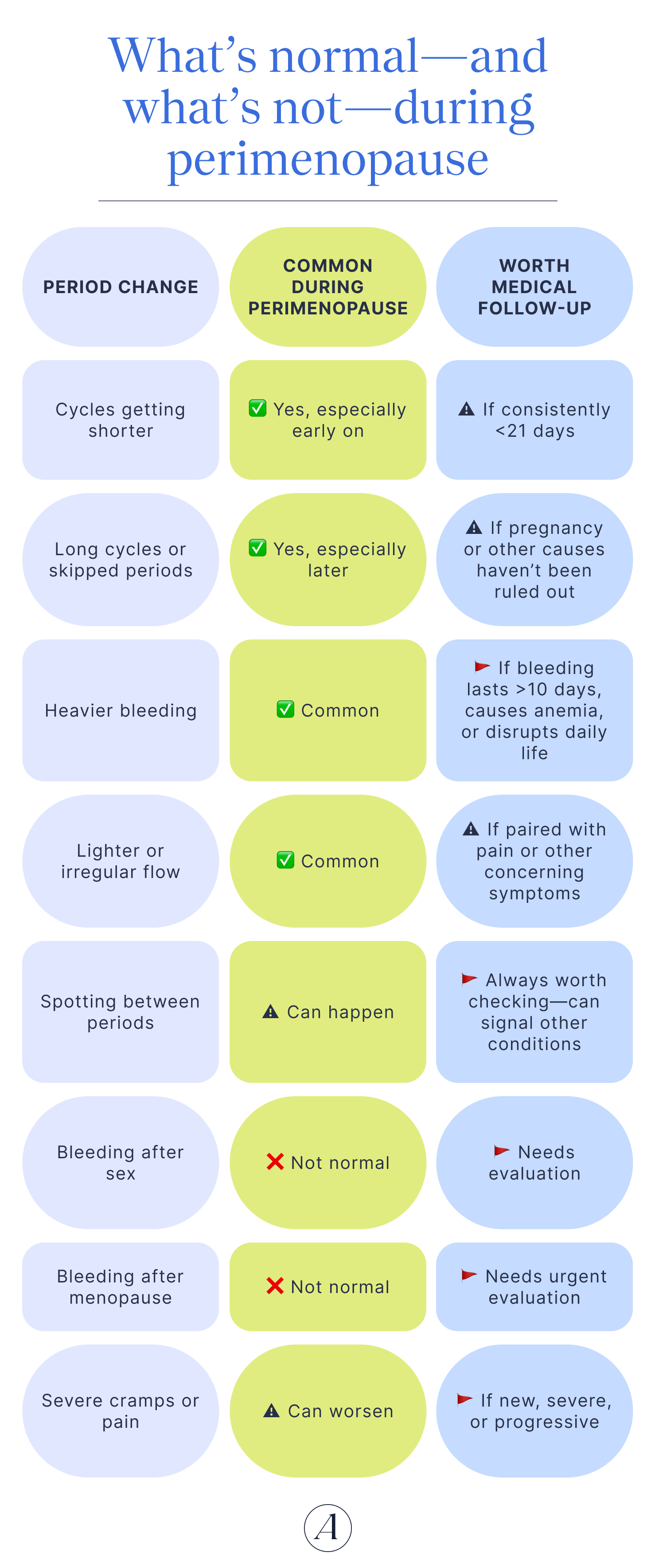
It’s completely normal for your cycle to change as you get closer to menopause, but that doesn’t mean you should ignore new or concerning bleeding. With all these shifts, it can be hard to tell what’s expected and what’s a red flag for periods during perimenopause.
Some changes are common. Others are your cue to call your ob-gyn. Dr. Pimputkar recommends medical evaluation if you’re dealing with:
- Bleeding that lasts longer than 10 days
- Very short cycles (less than 21 days apart)
- Heavy bleeding that leads to anemia or symptoms like fatigue or shortness of breath
It’s also not considered normal to have:
- Bleeding or spotting between periods
- Bleeding or spotting after sex
- Any bleeding after menopause
And periods aren’t the only reason to seek help. If perimenopause symptoms start affecting your quality of life, it’s time to talk to a provider, says Dr. Pimputkar. That includes mood shifts, low energy, hot flashes or night sweats, vaginal dryness, low libido, or painful sex.
Other conditions that can affect your period
“There are many other health conditions that can affect a woman’s period during this time,” says Dr. Pimputkar. Some issues can mimic perimenopause, overlap with it, or hide something more serious. Possible causes of abnormal bleeding include, per Dr. Pimputkar:
- Uterine issues, like fibroids, polyps, or cervical dysplasia (a precancerous condition linked to HPV)
- Hormonal or metabolic conditions that disrupt ovulation, such as thyroid disorders, polycystic ovary syndrome (PCOS), high prolactin levels, or obesity
- Endometrial hyperplasia (a condition that makes the uterine lining too thick, which can lead to cancer) or uterine cancer
And yes—pregnancy still belongs on the list, says Dr. Pimputkar. Even with irregular cycles, ovulation doesn’t stop during perimenopause; it just becomes unpredictable. In fact, hormone fluctuations can trigger multiple ovulations close together, which helps explain why the odds of spontaneous twin pregnancy double by age 35 and triple by age 40.
The takeaway? If your period changes, don’t guess—get checked. Seeing your provider is the smartest way to separate normal perimenopause shifts from something that needs treatment.
How to track and manage perimenopause-related period changes
If your period has gotten unpredictable, heavier, lighter, or just plain confusing, the smartest first step is to track what’s actually happening. No high tech required—you can use an app or good old pen and paper. Some providers even use period-tracking charts like this.
The idea is to log info for each cycle. Note things like:
- How many days your cycle lasts
- How many pads or tampons you use per day (plus, how soaked they are)
- How many days you bleed
- Any clots
- Other symptoms like dizziness, fatigue, light-headedness, or intense cramps
Track this for a few cycles. This kind of detail helps your provider spot patterns, rule out other causes, and figure out whether perimenopause is the real culprit.
Once perimenopause is behind your period changes, the focus shifts to managing symptoms and supporting your body. The good news: there’s a lot you can do, starting with lifestyle habits and layering in medical care when needed.
Lifestyle supports
Small daily habits = big long-term payoff. “Lifestyle changes can help improve your period symptoms and set you up for success during perimenopause,” says Dr. Pimputkar. And the earlier you start, the smoother the transition tends to be.
Exercise
Regular physical activity helps ease both the physical and emotional changes of perimenopause, says Dr. Pimputkar. Exercise improves insulin resistance and central abdominal fat, which can worsen non-ovulatory cycles, she explains.
It also triggers the “release of powerful anti-inflammatory molecules in the body” that help stabilize blood sugar, “clear excess cholesterol,” and reduce systemic inflammation, says Felice Ramallo, MSCN, RDN, LD/CDN, lead dietitian at Allara Health.
Strength training deserves special mention. Estrogen plays a key role in bone and muscle health, and as it drops, bone density and muscle mass can take a hit, says Ramallo. Weight-bearing and resistance exercises help counteract those effects and preserve body composition, she says.
And let’s not forget mood: movement is a proven mood booster during hormone swings.
The goal:
- 150–300 minutes of moderate activity per week
- Strength training twice weekly
All movement counts. Take the stairs. Go for a walk. Add ankle weights or a weighted vest for an extra boost to bone health. Every minute adds up.
Sleep
Protect your sleep like it’s a non-negotiable—because it is.
“Our bodies need sleep to reset many of our metabolic processes,” says Dr. Pimputkar. Declining estrogen can directly disrupt sleep quality, making rest even more essential (and sometimes harder to get), she says.
Sleep-supporting basics, per Dr. Pimputkar:
- Stick to a consistent nighttime routine
- Cut back on screens before bed
- Keep your bedroom cool, dark, and quiet
- Go easy on alcohol—and caffeine
Stress management
Chronic stress ramps up cortisol, which can worsen insulin resistance and hormone dysregulation. Tools like meditation, yoga, and other mind-body practices help calm the stress response and can meaningfully improve perimenopause symptoms over time, says Dr. Pimputkar. You don’t need an hour of meditation either. Just a few minutes of intentional breathwork and mindfulness a day can be a great place to start.
Kick the habit
We can’t control our hormones, but we can control our behaviors, says Dr. Pimputkar. Smoking is a big one.
“Smoking has been associated with an earlier onset of menopause and increased severity of symptoms,” says Dr. Pimputkar. If you needed another reason to quit, this is it. And if you need help, support programs can make a huge difference. Start your smoke-free journey here.
Nutrition & diet
When we want to use our dietary choices to support cycle changes in perimenopause, “it comes down to the root of inflammation,” says Ramallo. “In this case, inflammation refers to dysregulation in the body … due to dropping female sex hormones.”
As estrogen drops, metabolic dysfunction can creep in—showing up as blood sugar issues, insulin resistance, rising cholesterol, and increased cardiovascular risk, she explains.
One of the best ways to keep these issues in check? A healthy diet. Start with these basics, says Ramallo:
- Follow a balanced plate: ½ fruits/veggies, ¼+ protein, up to ¼ high-fiber starches
- Prioritize whole, minimally processed foods
Some standout perimenopause MVPs, per Ramallo:
- Colorful fruits & veggies: Think “strive for 5” servings daily for antioxidants and anti-inflammatory benefits.
- Nuts & seeds: Flax, walnuts, chia, pumpkin seeds, and hemp hearts support heart and hormone health.
- Plant proteins: Beans clear excess cholesterol, balance blood sugars, and fight inflammation by feeding gut bacteria with prebiotic fibers. Soy—a cholesterol-free protein—is linked to fewer menopause symptoms. Protein, in general, is essential for preserving muscle and bone during estrogen decline.
- Vitamin D & calcium-rich foods: Dairy, fortified foods, nuts, seeds, and bony fish support bones and hormone production.
What to limit, per Ramallo:
- Added sugar: Can worsen hormone balance and cycle irregularity (aim for ≤10g per serving)
- Alcohol: Highly dysregulating—keeping intake under 1–2 drinks per day (or skipping it) can noticeably improve symptoms
- Caffeine: More than 2–3 servings daily may worsen symptoms for some people
Supplements
Under the guidance of a menopause-informed provider, certain supplements may help support cycles and symptoms, per Ramallo:
- Soy isoflavones: Support sex hormone balance, regulating cycles and reducing hot flashes
- Omega-3s: Excellent for hormone balance and cardiovascular health
- Vitamin D: Essential for hormone synthesis and regulation
- Inositol: Supports both sex hormones and insulin signaling
- Berberine & N-acetylcysteine (NAC): May help improve blood sugar regulation, especially impactful for people with insulin resistance
Medical treatments
Lifestyle supports are foundational, but sometimes symptoms need more backup. You don’t have to tough it out. According to Dr. Pimputkar, options include:
- Hormonal contraceptives (pill, patch, or vaginal ring): Help regulate heavy or irregular bleeding, reduce pain, relieve hot flashes, and provide contraception
- Progesterone-releasing IUD: Especially effective for heavy periods
- Menopause hormone therapy (MHT): Treat symptoms like hot flashes and vaginal dryness by replacing estrogen (and often progesterone).
- If you have a uterus, MHT includes estrogen plus progesterone
- Progesterone may also improve sleep and can be taken nightly or cyclically
Talk with your provider to decide what fits your symptoms, health history, and goals best. Perimenopause is a transition, but with the right tools, it doesn’t have to derail your life.
When to talk to a healthcare provider
As you get closer to menopause, it’s expected for your cycle to shift, but certain changes deserve a closer look. Reach out to a provider if you notice:
- Bleeding that lasts longer than 10 days
- Very short cycles (less than 21 days apart)
- Heavy bleeding that causes anemia or symptoms like fatigue or shortness of breath
- Bleeding or spotting between periods or after sex
These aren’t things to power through or brush off.
And it’s not just about what’s happening on your pad or tampon. If perimenopause symptoms start creeping into your daily life, that’s reason enough to speak up. Mood changes, low energy, hot flashes or night sweats, vaginal dryness, low libido, and painful sex can all take a real toll, and you don’t have to wait until things feel unbearable to ask for help.
When you do meet with a provider—whether that’s in person or through a virtual Allara Health appointment—having some concrete data can make the conversation much more productive. Bringing your period-tracking notes helps your provider identify patterns, rule out other causes, and better understand what’s behind your symptoms.
It’s also helpful to know that perimenopause doesn’t always show up neatly on a lab report. In fact, symptoms alone are often used to make the diagnosis. That’s because hormone levels fluctuate unpredictably during the transition to menopause, making blood tests an unreliable snapshot of what’s really happening in your body.
From there, the focus shifts to figuring out what support actually makes sense for you. Depending on what’s bothering you most—irregular periods, other symptoms, or both—you and your provider can talk through options like lifestyle changes, supplements, medical treatments, or a combination of the three. The goal is a plan tailored to your needs, health history, and priorities. And once that plan is in place, stay in touch. Perimenopause is a moving target, and regular check-ins allow your provider to fine-tune what’s working or pivot if it’s not.
The bottom line
Perimenopause periods can feel chaotic, frustrating, and honestly a little rude—but they’re also your body’s way of signaling a major hormonal transition. Understanding why your cycle is changing helps you take the guesswork (and fear) out of what’s happening and recognize when something deserves medical attention.
What matters most, you don’t have to white-knuckle your way through this phase. If your periods feel unmanageable, confusing, or disruptive, getting support can make a real difference. The experts at Allara will investigate, diagnose, and create a personalized treatment plan so you can get to the bottom of your symptoms and feel more in sync with your body again—on your terms.
Key takeaways
- Period changes are often the first sign of perimenopause. Shorter or longer cycles, skipped periods, heavier or lighter bleeding, and spotting are all common as hormones fluctuate and ovulation becomes less predictable.
- Some bleeding patterns are normal—but not all. Prolonged bleeding, very heavy flow, bleeding between periods or after sex, or bleeding after menopause should always be checked out.
- Tracking your cycle matters. Noting flow, duration, clots, and symptoms helps providers spot patterns, rule out other conditions, and tailor treatment.
- You have options. Lifestyle changes, supplements, and medical treatments can all help manage perimenopause periods—you don’t have to just wait it out.
Frequently asked questions (FAQs)
What are the common symptoms of perimenopause?
One of the earliest—and most common—signs is changes in your menstrual cycle. Periods can suddenly get shorter, longer, heavier, lighter, more frequent, delayed, or show up with surprise spotting, says Dr. Pimputkar.
But wonky periods aren’t the only clue you’re experiencing perimenopause. Many people also notice other symptoms, including:
- Mood changes
- Changes in sex drive
- Brain fog or memory lapses
- Headaches
- Night sweats or hot flashes
- Vaginal dryness
- Sleep problems
- Joint or muscle aches
- Heavy sweating
- Needing to pee more often
- PMS-like symptoms
Still, no two people will have the same perimenopause experience. If something feels off—or starts interfering with your life—it’s worth talking to a provider. You don’t have to tough it out.
How is perimenopause diagnosed?
Most of the time, the diagnosis comes down to symptoms—not blood tests. Hormone levels swing wildly during the menopausal transition, so a single lab value often doesn’t reflect what’s really happening. Because of that, providers usually rely on your symptoms, cycle history, and overall picture rather than labs alone.
What is the average age for perimenopause?
Perimenopause typically begins in the mid- to late 40s, though it can start earlier for some people. It can last anywhere from two to eight years before periods stop completely and menopause officially begins.












